


SEE THE WINNERS
& DOWNLOAD
THE COLORING BOOK!
WORLD DIABETES DAY
14TH NOVEMBER
2025
DIABETES
IMAGES
OF THE YEAR
Thank you to everyone who took part in the 2025 This Is Diabetes, This Is Anxiety
Art Competition.
We are proud to present the winning entries, chosen by Ascensia Diabetes Care
and our expert judging panel, from submissions received across 25
countries. Each piece tells a powerful story about diabetes and mental wellbeing,
helping raise awareness and empathy across the global community.
Explore the winning artworks below, download our free coloring book inspired by
selected entries, and take part by coloring and sharing your creations on social
media using #WDD2025 #ThisisDiabetes.
1ST PRIZE

Emmanuel Moreno Lopez
Almost at the Limit
Mexico
Donation will be made to charity:
Asociación Mexicana de Diabetes
CLICK TO READ THE STORY
2ND PRIZE

Irene Cotroneo
So little, so big
Italy
Donation will be made to charity:
Fondazione Italiana Diabete
CLICK TO READ THE STORY
3RD PRIZE
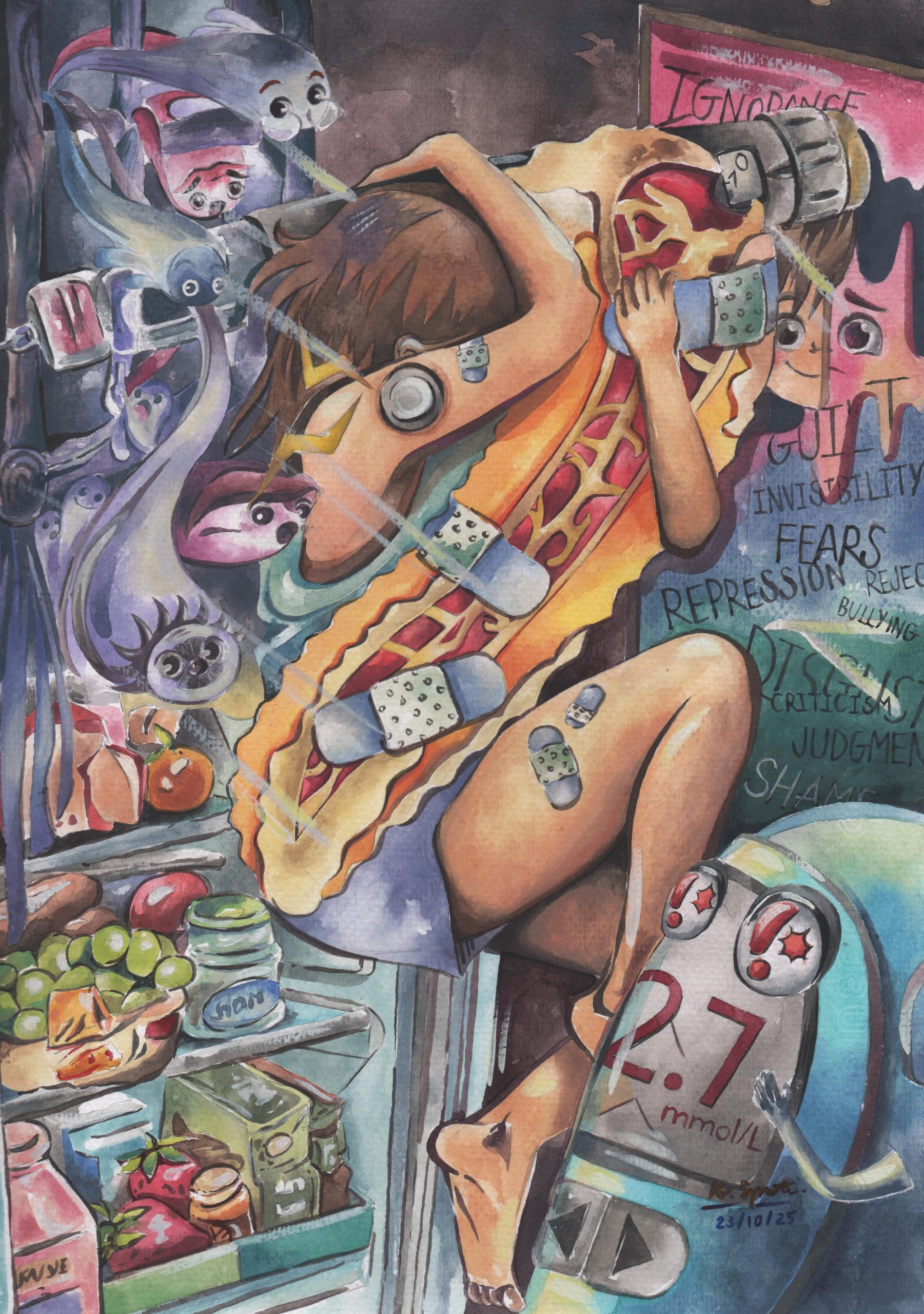
Kanjaree Suppawittaya
The Quiet Courage
Thailand
Donation will be made to charity:
Diabetes Association of Thailand
CLICK TO READ THE STORY
2025 SELECTED SUBMISSIONS GALLERY

Belma Tahto
Invisible Weight
Bosnia and Herzegovina
click to view the story

Nawelles La Rosa
The Voices Within
Italy
click to view the story

Diego Berzagui
Rebirth from Darkness
Brasil
click to view the story

Linda Chan
Bad hair day lady
United Kingdom
click to view the story
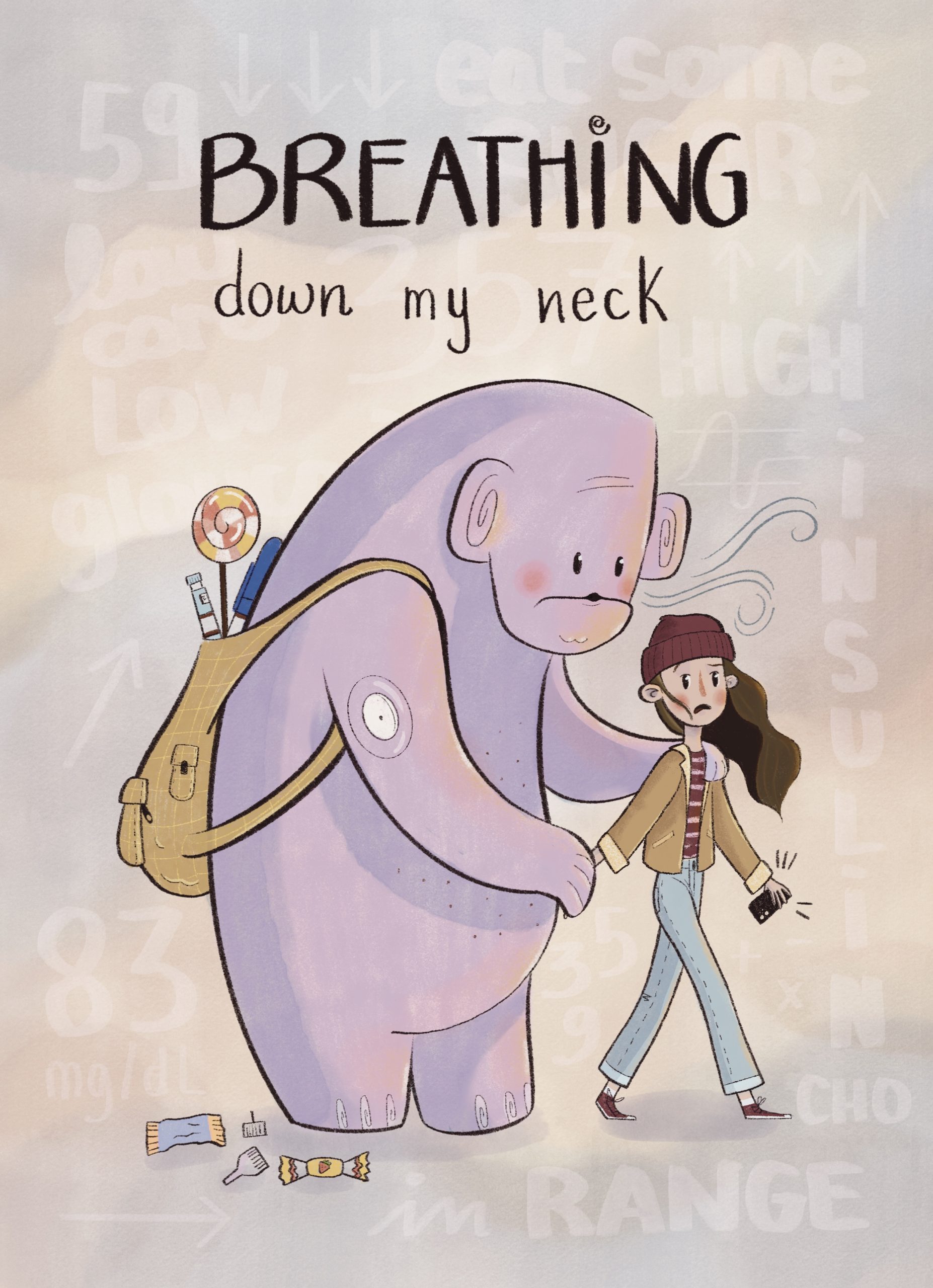
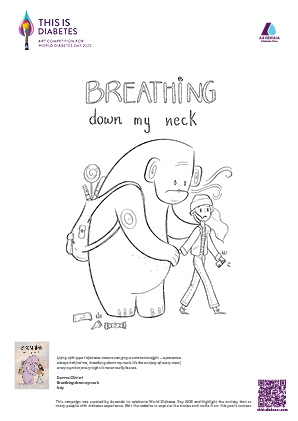
Gemma Olivieri
Breathing down my neck
Italy
click to view the story

Lynda Browne-Bristov
Still, I Grow (With Insulin)
Barbados
click to view the story

Isabelle Isa Kristin Steineck
The diabetes parent
Sweden
click to view the story

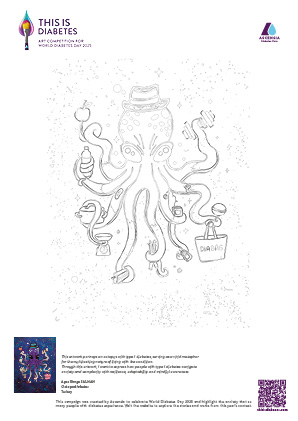
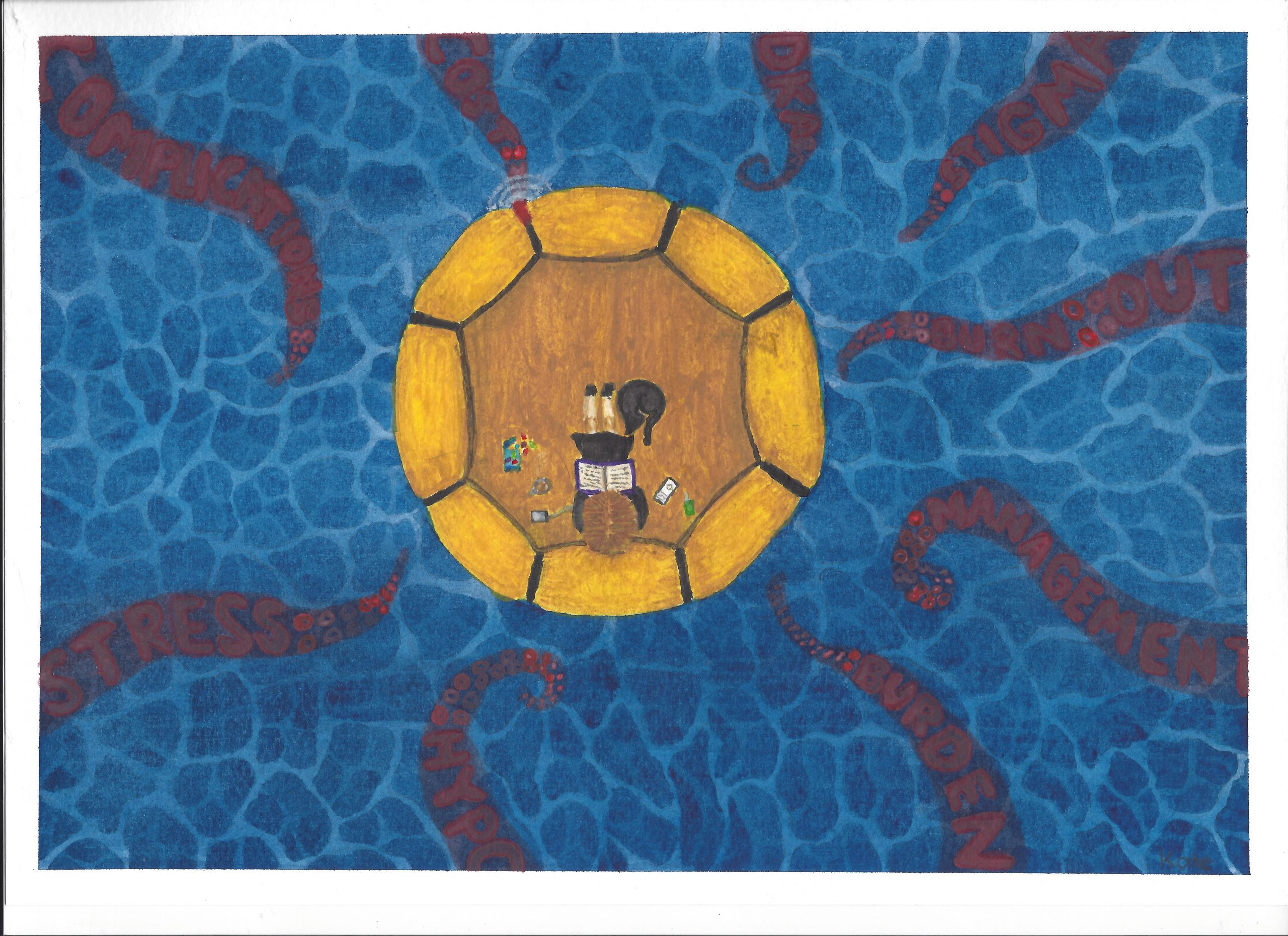
Ayse Simge Salman
Octopodiabetes
Turkey
click to view the story
Kate Mirosevich
Anxiety from the Depths
Australia
click to view the story

Cristiano Da Silva
Engulfed in Blue
Canada
click to view the story

Lorena De Leo
Anxiety and Her Friends
Italy
click to view the story
Haley
(Not So) Imaginary Monsters45r
United States
click to view the story
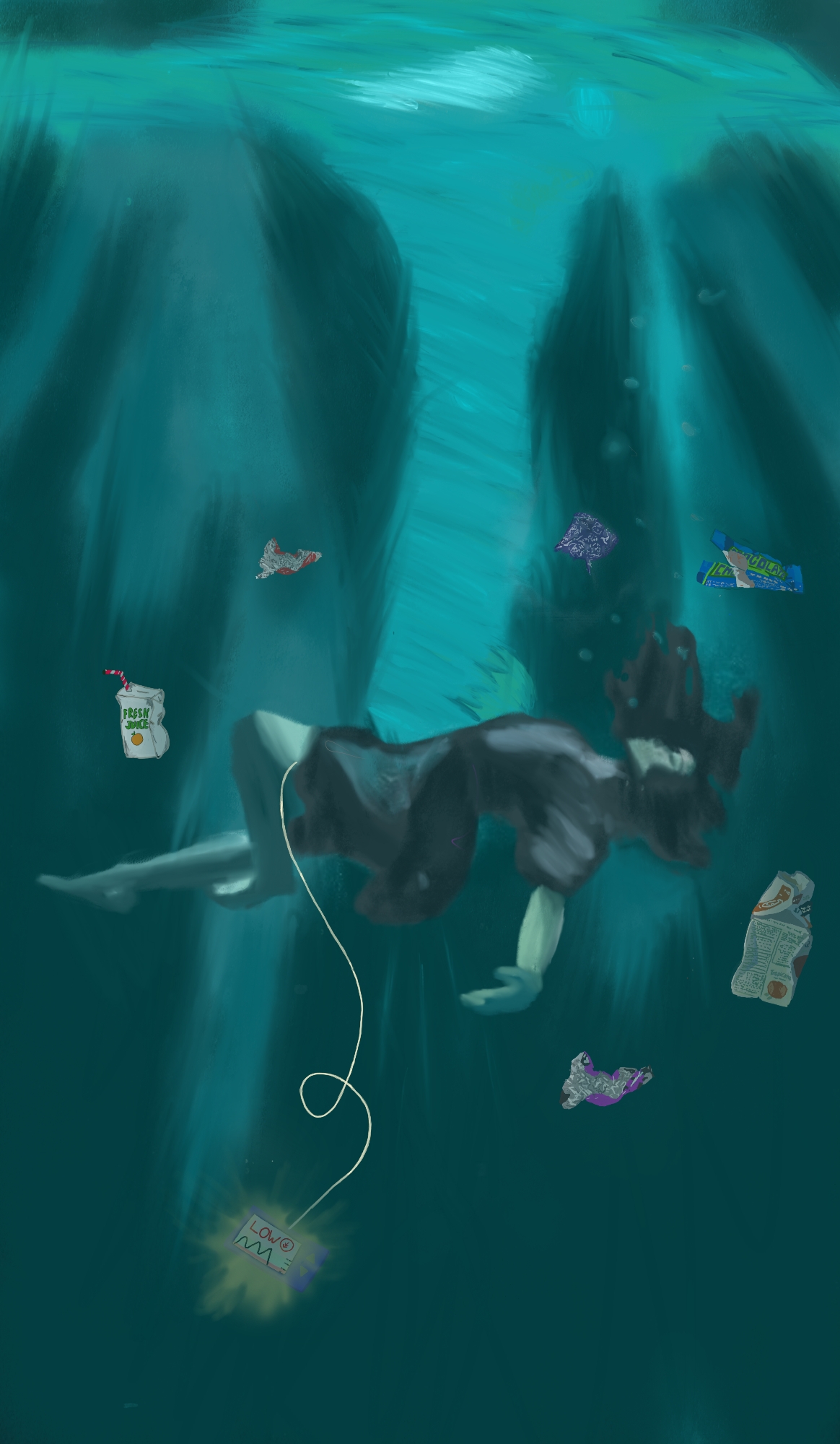
Hannah Böhm
Drowning
Germany
click to view the story
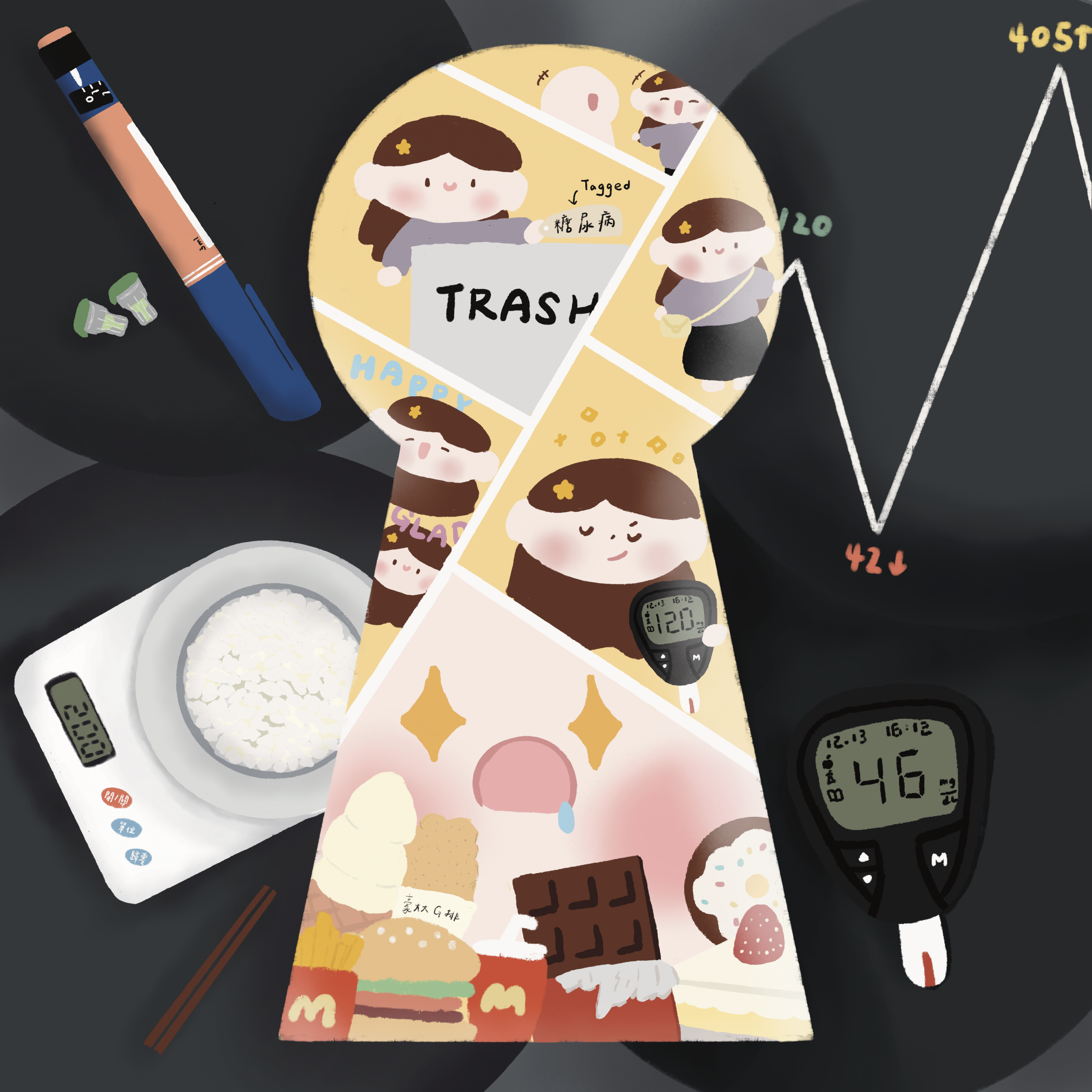
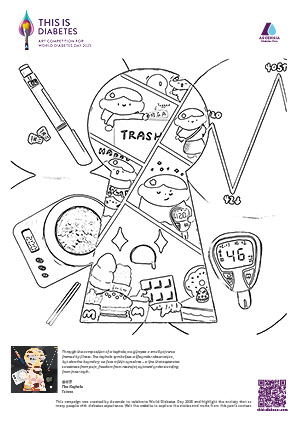
林宇芹
The Keyhole
Taiwan
click to view the story

Sara Mariana Meléndez Barrón
To My Dear Pancreas and Brain
Mexico
click to view the story

Jaylen MM
Is This Me?
Canada
click to view the story

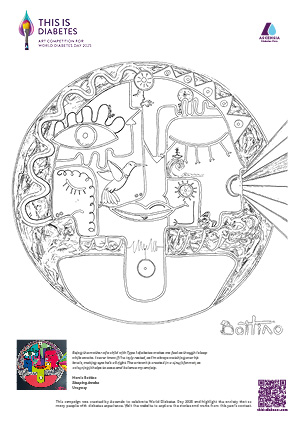
Marcia Bottino
Sleeping Awake
Urugway
click to view the story
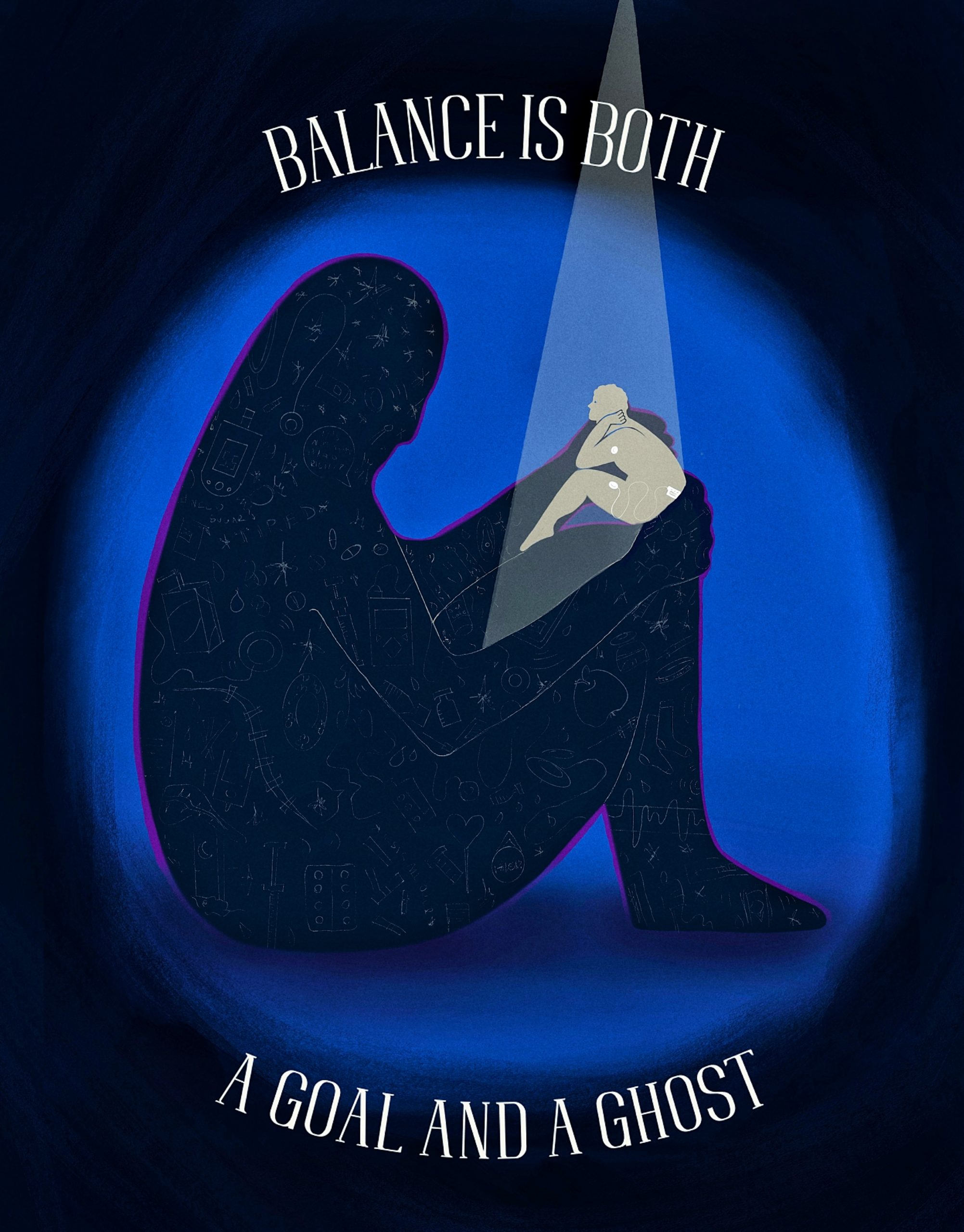
Stefanie Hilbeck
Wrapped in Worry
Germany
click to view the story

Marwa Kicha
Through the Tunnel of Struggle
Morocco
click to view the story

Sharron Fidler
Say cheese! A portrait of my social anxiety
United Kingdom
click to view the story

Louise Richardson
Tip of it
United Kingdom
click to view the story

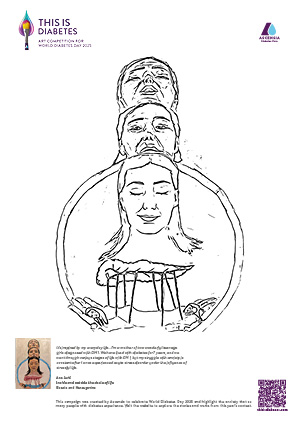
Ana Jurić
Inside and outside the circle of life
Bosnia and Herzegovina
click to view the story

Ariadna Castrellón Calzada
Diabetes labyrinth
Mexico
click to view the story

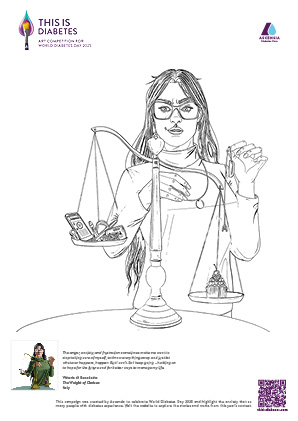
Vittoria di Benedetto
The Weight of Choices
Italy
click to view the story

Chloe Moon
Tragically Beautiful
Australia
click to view the story

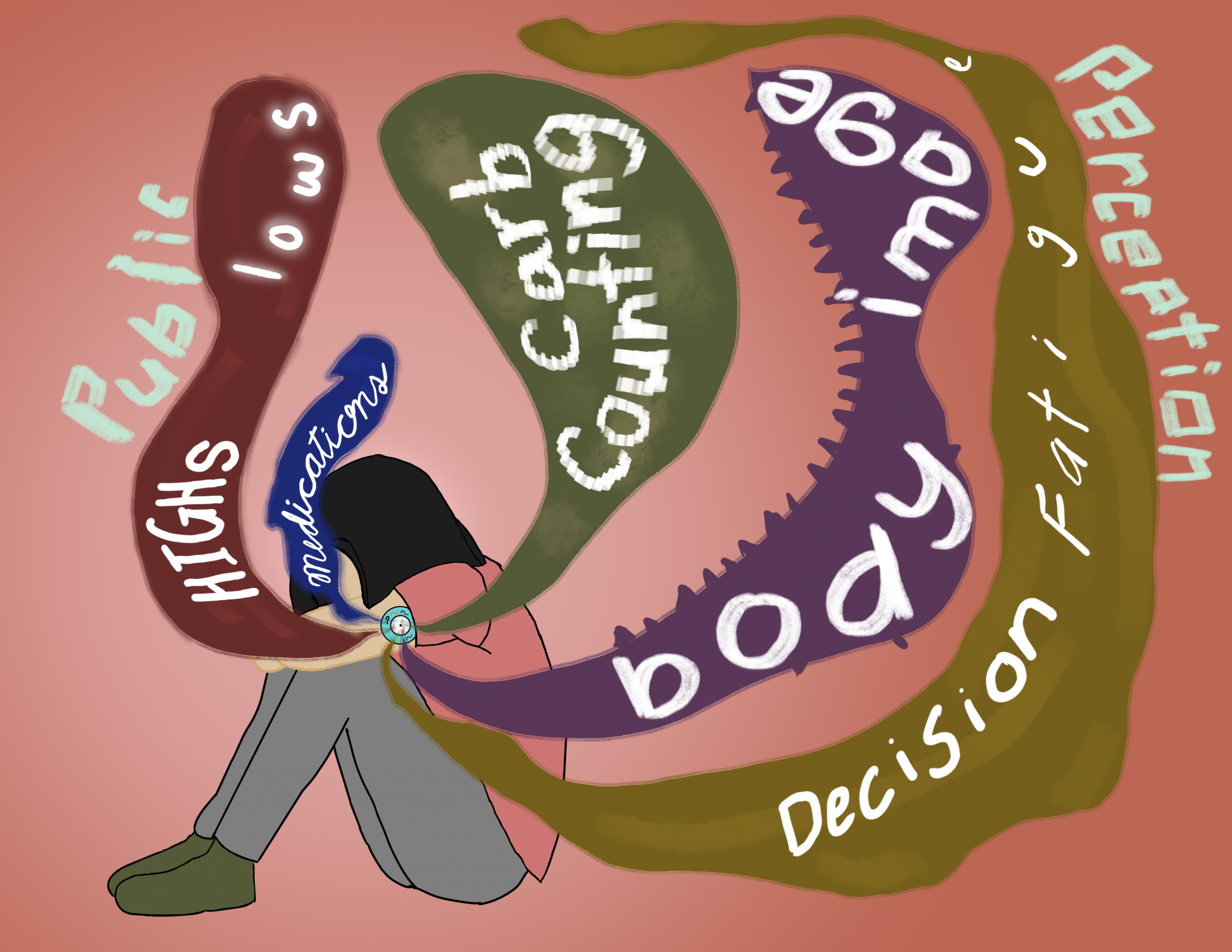
Shelby Dillingham
Tread Lightly (This Is Anxiety)
United States
click to view the story
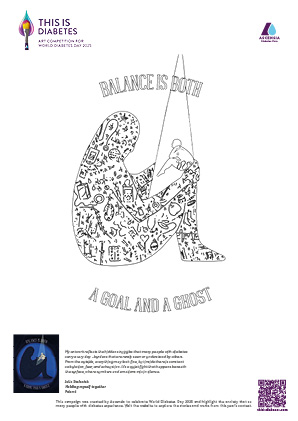
Julia Stefaniak
Holding myself together
Poland
click to view the story

Francesco Pecchia
Fragile Silences
Italy
click to view the story

Ingo Vieweg
Colour Flash
Germany
click to view the story

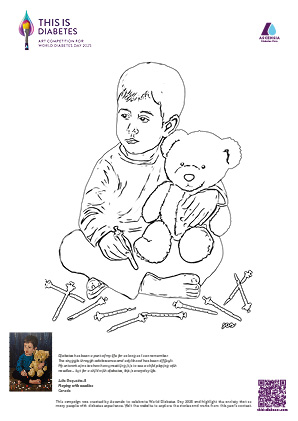
Julie Duquette-B
Playing with needles
Canada
click to view the story

Nina Emmerich
Silent Cry for Help
Germany
click to view the story

Roberto Carlos Velazquez Zamora
Within Me
Mexico
click to view the story
Daniela Asparuhova Georgieva
The Battle Within
Switzerland
click to view the story
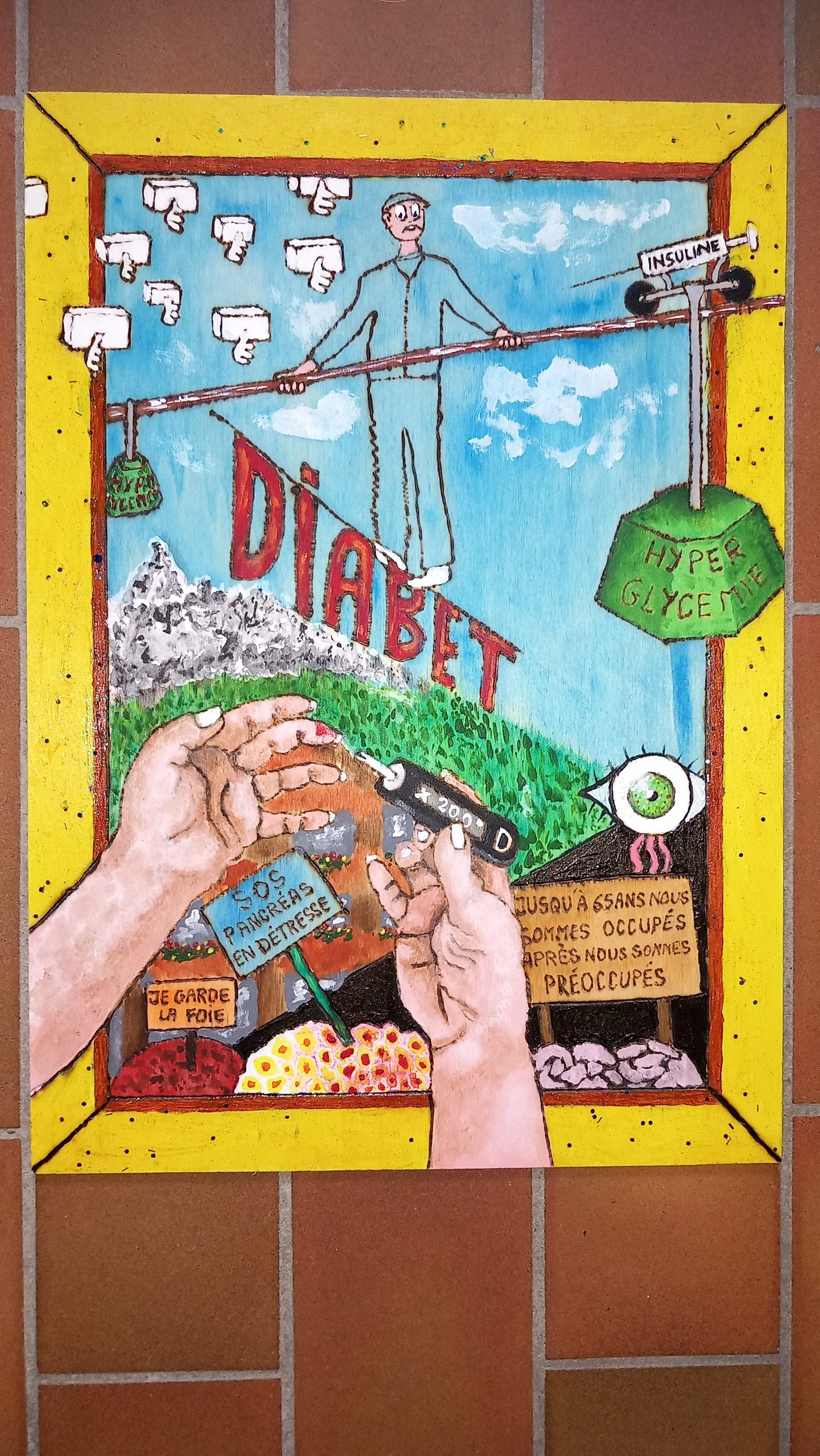
Kongchai Bernard
Diabetes Is a Matter of Balance
Switzerland
click to view the story

Almost at the Limit
Emmanuel Moreno Lopez, Mexico
This work is born from a deeply personal place: my father and my grandparents lived with diabetes. Growing up watching how they dealt with those numbers every day, with that silent stress, left a mark on me. Their experiences became both an inspiration and a reminder that the battle is fought not only in the body but also in the mind.
“Almost at the Limit” seeks to visually represent the constant anxiety many people with diabetes feel when monitoring their glucose levels. The composition uses overlapping faces and hands to convey confusion, mental pressure, and the feeling of being trapped in multiple thoughts at once. This fragmentation reflects how the mind divides itself among fear, worry, frustration, and self-control.
The dramatic use of red and blue symbolizes two opposing forces: red as alert, stress, and urgency, while blue suggests calm, control, and clinical detachment. These opposing energies collide within the patient, representing the inner conflict that arises even before seeing the result.
At the center, the glucometer displays a reading of 127 — a number technically within the normal range, yet very close to the threshold. That closeness creates a real and persistent anxiety: the fear of being just about to go wrong. For many people with diabetes, every measurement can trigger thoughts of guilt, frustration, or fear of losing control. The device thus becomes an emotional symbol, not merely a medical one.
The multiple hands emphasize the repetitive, almost compulsive action of testing — a necessary routine, but one that drains the mind. The fragmented face represents the patient’s emotional identity: outwardly composed, but inwardly divided by worry.
With this piece, I aim to express that anxiety in people with diabetes doesn’t always come from bad results, but from the constant possibility of crossing that line. Living “almost at the limit” is a mental state — a daily reminder that even the slightest variation can bring serious consequences. This work invites empathy, understanding, and a visualization of that invisible pressure.
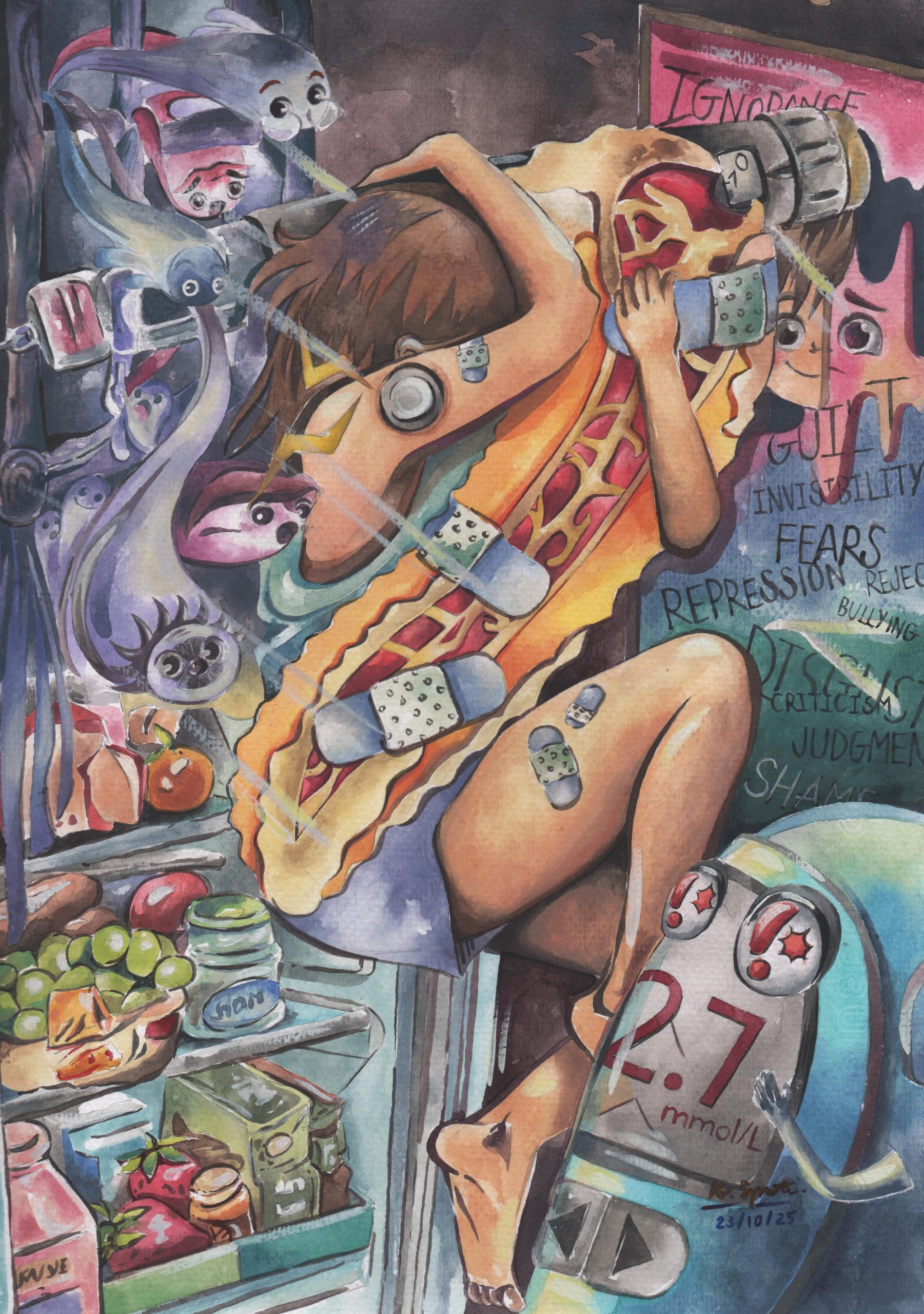
The Quiet Courage
Kanjaree Suppawittaya, Thailand
Living with Type 1 Diabetes comes with an invisible weight — as a T1D patient for over ten years, I have come to the realization that perfect control every day is nearly impossible. Being constantly aware of keeping our blood sugar level in check, injecting the right doses of different types of insulin, managing high and lows, and making hundreds of other diabetes-related decisions — on top of all the normal decisions everyone makes daily — create a feeling of “never being off duty” and an anxiety that comes from within.
While I have gained immense support from my family, peers, and healthcare team, there are still moments when I faced social situations and the pressure of eyes and ears that do not understand. I am grateful to be able to share my T1D story, but the need to constantly explaining myself to everyone who sees my conditions — hoping deeply that they will understand, and sometimes letting it pass for those who do not — is overwhelming. Others’ misconceptions and hurtful predictions about my future are often painful and sometimes make me feel uncertain despite having a lot of faith and confidence in myself and my abilities.
Ultimately, living with T1D is not just about managing numbers — it is about finding balance, resilience, and acceptance. For me, my first step was embracing all of who I am and saying to myself, “Yes, I have diabetes, and I will live well with it.” And that is exactly what I have done up until now. Being a patient myself and seeing what many may do not shaped me into a hardworking and empathetic third-year medical student today. I still carry some fears, but I know the strength within me and the support of our worldwide diabetes community will help me overcome anything. I hope to live a life well-lived, for the little 10-year-old me and for all of you, my dearly loved friends.

So little, so big
Irene Cotroneo, Italy
Every time I look at my insulin pump cart, I think about the fact that it is an incredibly small element that keeps me alive. So small and fragile but so big and necessary. Big because it is my first need and it is the second main character of my life, after myself. Sometimes I feel like there is no way out and I panic. Sometimes diabetes is just an ordinary task. I often struggle, but I keep on going. It is how it is.

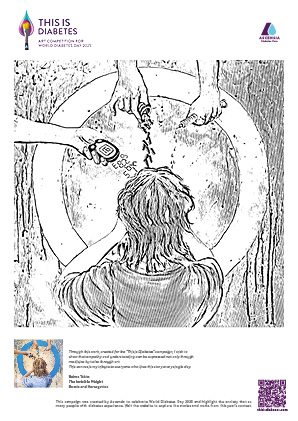
Invisible Weight
Belma Tahto, Bosnia and Herzegovina
My story of diabetes.
As a pharmacist, I meet people living with diabetes every day. Every conversation, every question, fear, or hope they share leaves a mark on me.
Over time, I learned that diabetes is not only a physical condition, but also an emotional journey, one that demands courage, patience, and resilience. As a self-taught painter, I try to turn these emotions into colors. This is how my art was actually born. It’s a visual expression of diabetes and anxiety, a blend of darkness and light, struggle and hope. It reflects the unseen side of diabetes, the anxiety, the invisible weight of uncertainty, but also the light of hope that never fades.
So, whether through my work as a pharmacist or through colors and brushstrokes, my mission remains the same: to help, to understand, and to offer support.
Through this work, created for the “This is Diabetes” campaign, I wish to show that empathy and understanding can be expressed not only through medicine but also through art.

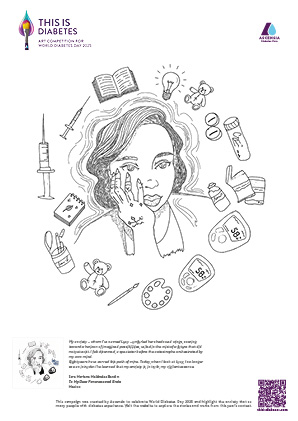
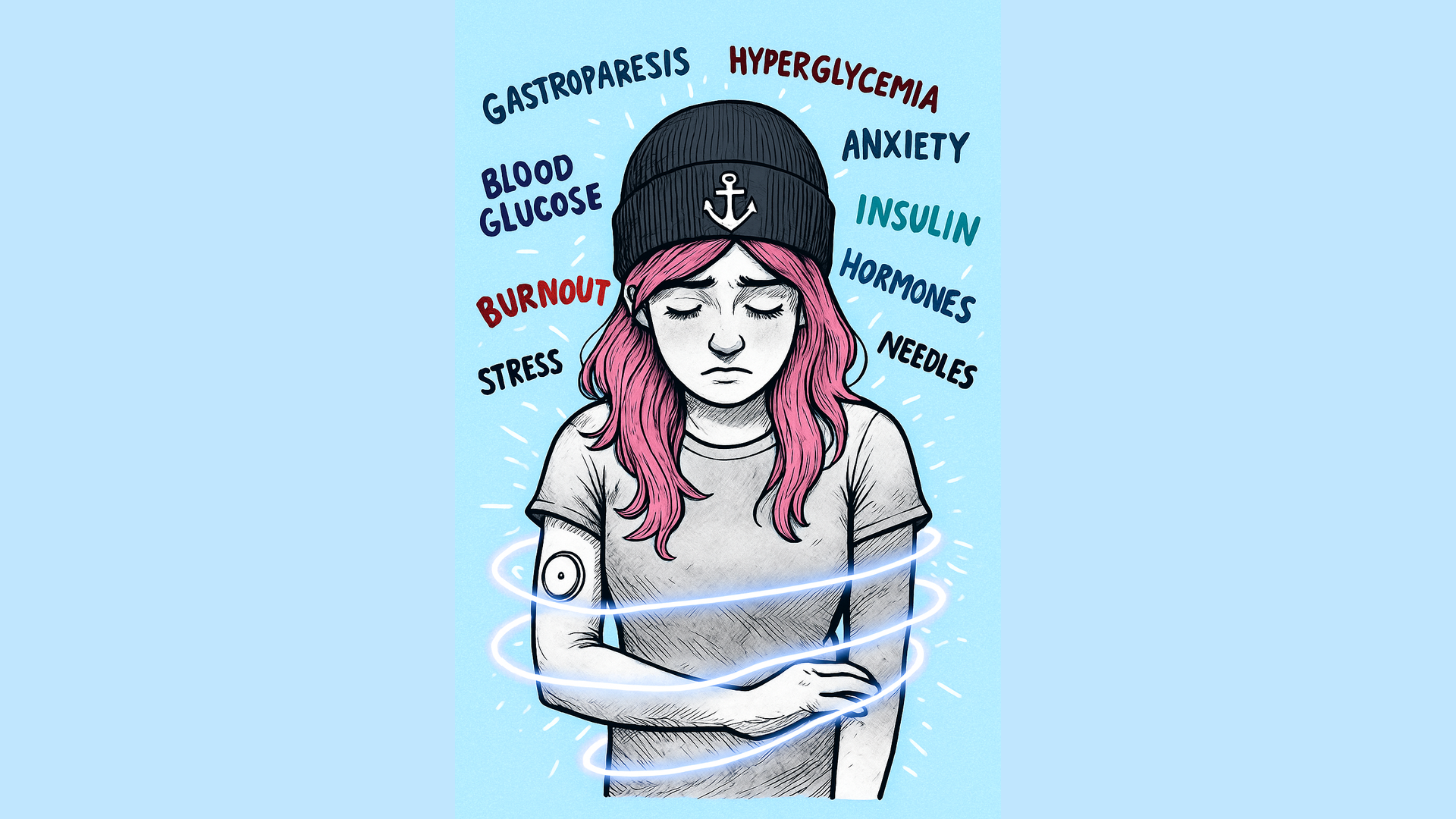
The Voices Within
Nawelles La Rosa, Italy
“The Voices Within” was born from silently listening to those who live with diabetes every day. Behind every act of control lies a universe of thoughts, anxiety, and fragile balance. It is a tribute to those who, in silence, face their battle — transforming pain into courage and awareness.
This artwork reflects the inner dialogue of those living with diabetes, a condition that extends beyond the body and reaches into the mind. The voices emerging around the face symbolise the constant anxiety of control, the fear of sudden changes, and the fatigue that comes from always having to stay alert.
In the calm, lucid face at the centre, we see the quiet strength of those who choose, day after day, to face their condition with awareness and dignity.The contrast between darkness and light expresses the inner path between emotional chaos and the search for balance.
It is an invitation to look beyond the illness — to recognise the invisible yet profound struggle that many endure, and to transform fear into resilience.

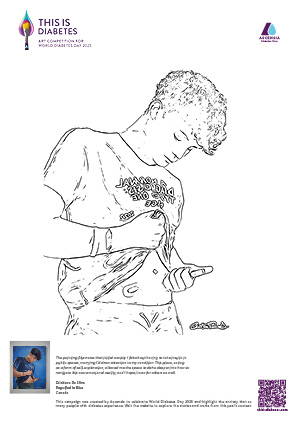
Rebirth from Darkness
Diego Berzagui, Brasil
“Rebirth from Darkness” portrays the journey of those who live with diabetes, the initial darkness, the fear and pain reflected in the eyes, but also the explosion of colour that bursts from the mind when one discovers it is possible to live fully. The heart on the chest symbolises love that endures, even in the face of limitation, while the organic shapes emerging from the head represent hope, discipline, and the blossoming of a new life.
The artwork reminds us that diabetes is not an ending, but an invitation to reinvent oneself, to be nourished by awareness, and to be reborn in colour, balance, and vitality.

Bad hair day lady
Linda Chan, Bad hair day lady
Diabetic for 33 years, I am losing my sight. I retired due to depression and poor health at 55. I took art classes and now make marks and see images within them. Having a bad hair day is when things aren't going well, feeling that the hair or in this case, the diabetes, is the only thing that defines you due to the constant need to manage this condition and the constant effort, awareness and sadness that can overwhelm, no matter how hard you try.
Diabetes has caused me sight loss, heart issues, kidney disease and neuropathy as I have needed insulin in all that time....I now have a constant monitor and this is changing my life.
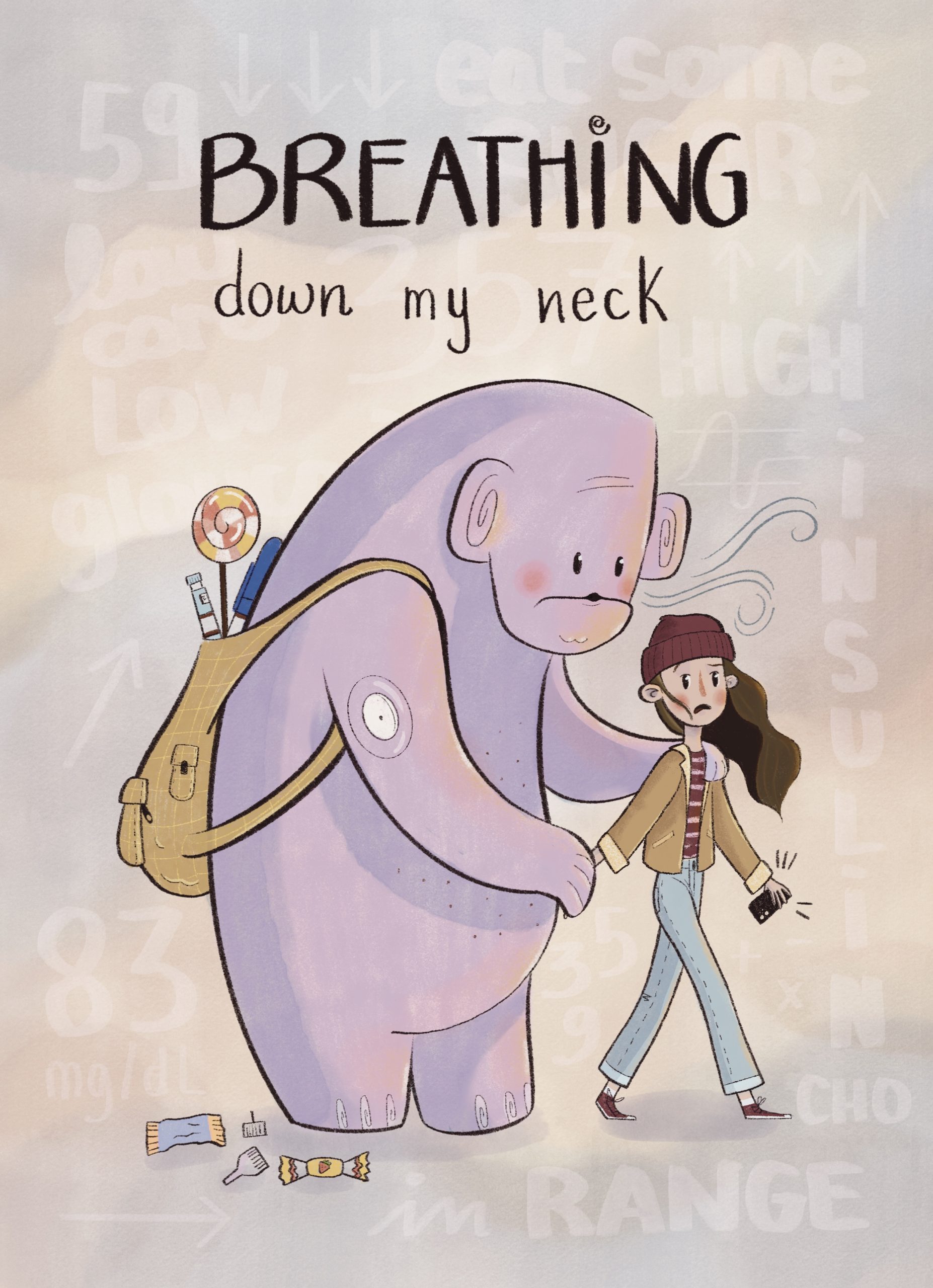
Breathing down my neck
Gemma Olivieri, Italy
Living with type 1 diabetes means carrying a constant weight — a presence always behind me, breathing down my neck. It’s the anxiety of every meal, every number, every night. It never really leaves.
I’ve been living with it since 2019 and I still hate it most of the time. It feels invasive, heavy — something that steals my freedom and fills every moment with worry. It drives me mad sometimes, this constant breath reminding me that I’m never completely free.
But I know I can’t go back. The only way forward is to keep walking, with it right behind me. Not as an enemy, but as a stubborn travel companion — one I’m slowly learning to live with, one breath, one step at a time.

Still, I Grow (With Insulin)
Lynda Browne-Bristov, Barbados
Diabetes has taught me to live alongside a low hum of anxiety, the numbers, the needles, the what-ifs, the highs and the lows. In this self-portrait, I reach with one hand and steady with the other, holding a staff of sugar cane that blossoms into a flower. The bloom is growth, softness and hope; the staff is resolved. An insulin pen rests at my hip, a constant reminder of my plight, but also a companion that subdues fear so I can keep moving forward with positivity.

The diabetes parent
Isabelle Isa Kristin Steineck, Sweden
Imagine having to give your child a medication every single day—knowing that too much of it could be dangerous, and too little could be life-threatening. This is the daily reality for parents of children living with type 1 diabetes.
Managing insulin is a complex and relentless task. Behind every dose is careful calculation, constant monitoring, and deep concern. And while carrying this medical responsibility, these parents are also simply trying to be ordinary moms and dads.
As a doctor, I meet many of these parents in my work. That’s why I wanted to create this drawing—to honor what they do. I also live with type 1 diabetes myself, and when I was a child, it was my own parents who shouldered that enormous burden for me.

Octopodiabetes
Ayse Simge Salman, Italy
This artwork portrays an octopus with type 1 diabetes, serving as a vivid metaphor for the multitasking nature of living with the condition. Each of the octopodiabetes's eight arms holds a diabetic device, symbolizing the constant balancing act and mental load that come with managing type 1 diabetes. Octopodiabetes wears a blue hat and floats in a space-like background. The blue hat not only represents T1DM awareness but also references the ''Blue Hat'' from the Six Thinking Hats Teaching Technique, a symbol of organization, reflection, and control over the thinking process.
I believe that type 1 diabetes has taught me a lot since my childhood. Today, as a teacher, I feel like I must teach my students and other people what type 1 diabetes is, and what it is not, to raise awareness, especially when they ask about my diabetic devices. Through this artwork, I want to express how people with type 1 diabetes navigate anxiety and complexity with resilience, adaptability and mindful awareness.
'One morning, when I wake up from my troubled dreams, I found myself transformed in a space into a versatile octopus.'' (A rephrased reference to Franz Kafka's The Metamorphosis*)
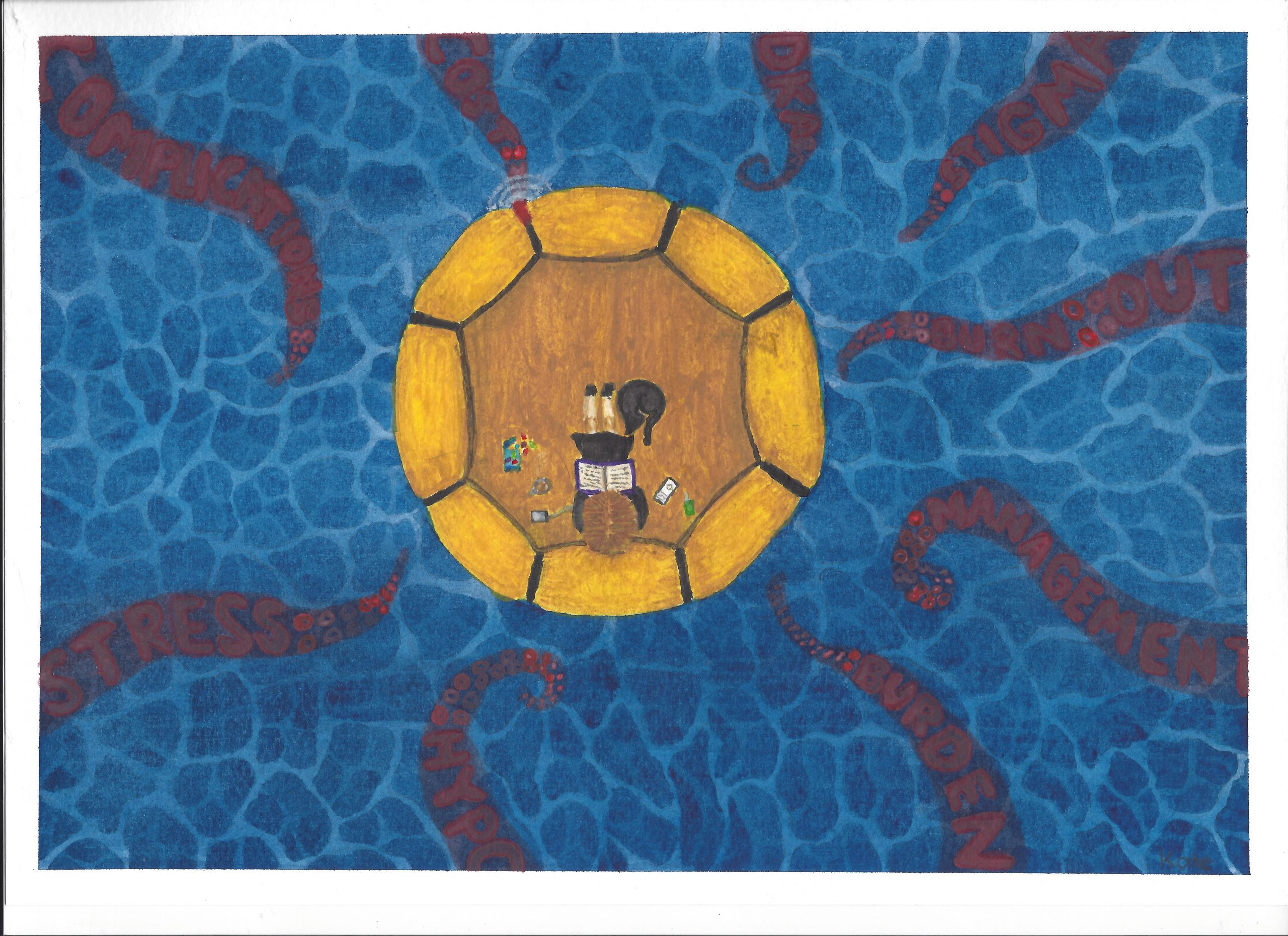
Anxiety from the Depths
Kate Mirosevich, Australia
The story behind this piece of art is that we are on a lifeboat and the lifeboat contains diabetes and everyday life and there is a balance.
Around the lifeboat, is the causes of anxiety that are lurking in the depths, inching closer. Some are just in the background and not making an impact on everyday life. However, sometimes these tentacles can reach the lifeboat and take hold of you. When it takes hold, the balance is broken and the things in life that are important can no longer be enjoyed the way they should be, not always visible to the world around us, but the effects can be great.
The tentacles are not always permanent, and they are not always making an impact, but they are ready to take hold again.

Engulfed in Blue
Cristiano Da Silva, Canada
Oil on canvas
18x24
The self-portrait "Engulfed in Blue" depicts me taking my bolus insulin injection, with a CGM on my right abdomen and a medical bracelet on my wrist. I was hospitalized after a month of overlooking my symptoms because I had a fear of being weak for not recovering on my own. With my diagnosis came both clarity and a life-altering reality.
The painting illustrates that initial anxiety I felt about having to take insulin in public spaces, worrying I’d draw attention to my condition. I chose the rich blues to represent the colour for diabetes awareness, with thick and blurred brush strokes to represent the chaos and ambiguity of how I felt in that moment.
I am often anxious about whether I am managing my condition correctly, to which I am grateful for the technology that helps make this process less worrying.
This piece, acting as a form of self-exploration, allowed me the space to delve deeper into how to navigate this new emotional reality, and I hope it can for others as well.

Anxiety and Her Friends
Lorena De Leo, Italy
I am the mother of a ten-year-old girl who was diagnosed with Type 1 diabetes at the age of seven. I created this artwork during 2024–2025, after two years of managing the condition through multiple daily insulin injections.
The greatest challenge was that I never received any training on carbohydrate counting or on the correct insulin-to-carbohydrate ratios. In practice, her treatment was based on observing each meal in relation to the insulin units administered and making corrections when needed. Over these two years, my mind became completely absorbed by experimenting with different combinations of foods and nutrients and watching the results.
Fear, mistakes, anger, confusion, exhaustion, and anxiety crowded my thoughts. From this came the need to face these emotions through drawing, to stop myself from being overwhelmed by them. Art, as therapy, gradually helps to clear the mind — it teaches you to ask for help, change hospitals, and seek proper training.
These are the right steps to take to see the light at the end of the tunnel and to find hope again.
In the end, my graphic works took the form of an artist’s book — what better way to represent the long, suffocating period spent at the mercy of these emotions?
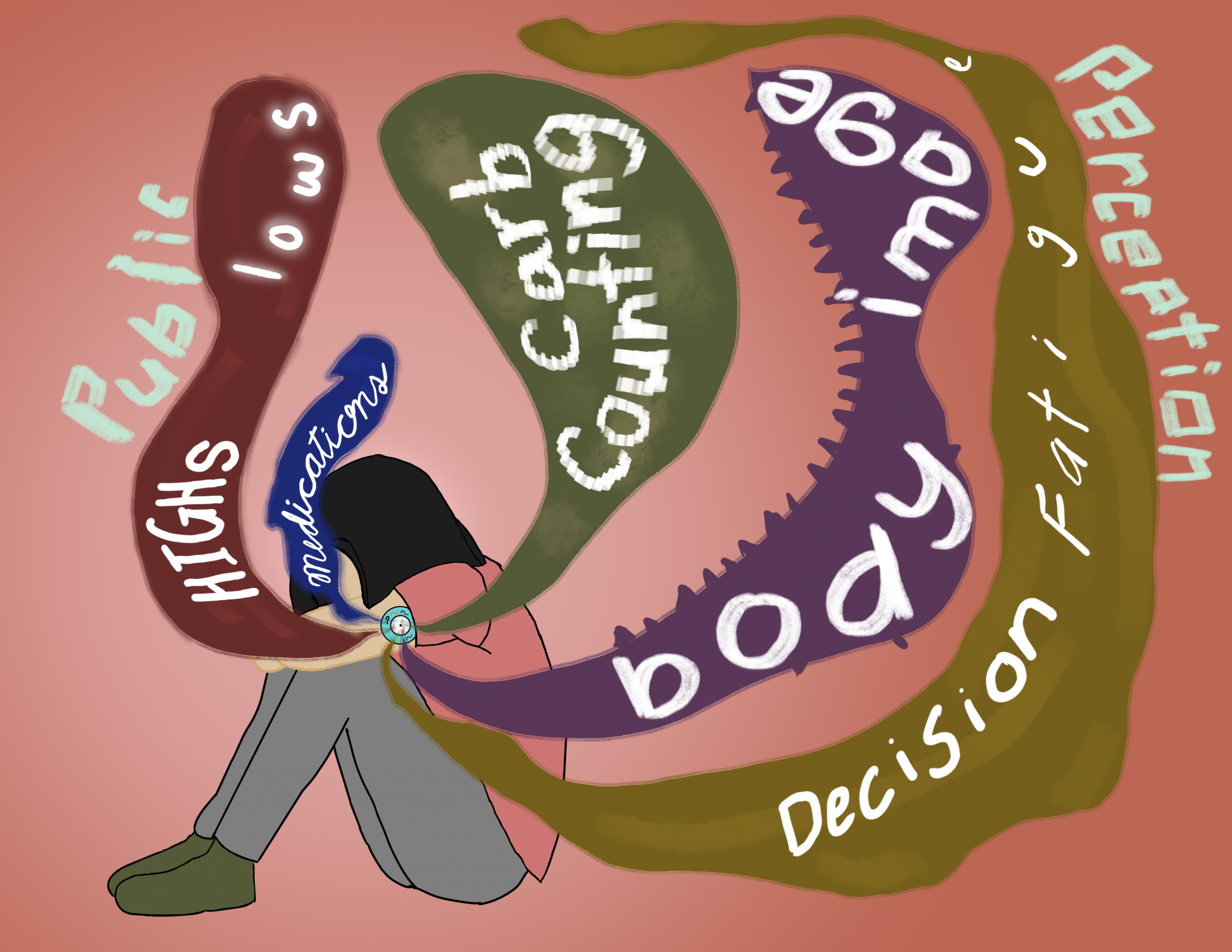
(Not So) Imaginary Monsters45r
Haley, United States
I have always been an anxious person—the kind of person who overanalyzes everything. I had my first panic attack when I was 13 and struggled with my anxiety throughout my adolescence. My anxiety was finally improving when I was diagnosed with diabetes at the age of 20. I was diagnosed at a hospital and it was all so overwhelming. I was given conflicting treatment plans, dealing with healthcare professionals who did not seem to know how to approach me, and no one could give me an answer on what type of diabetes I had. My anxiety skyrocketed.
I had reached a point when I entered adulthood where I was not thinking about each decision I made in a day. Diabetes changed that. Suddenly I had to consider my sugar levels any time I ate, exercised, or slept. I had to think if there were sharps disposal containers nearby. I had to remember insulin and daily pills for the first time in my life.
Receiving an official diagnosis helped relieve some of my anxiety, but that was replaced by a new anxiety. I am neither T1D or T2D, I have Maturity Onset Diabetes of the Young. There is limited research on MODY, and most people – even other diabetics – have never even heard of it.
This piece is a visual representation of my diabetic-induced anxieties. At times, it feels as if these worries are pressing in around me, that they are larger than me. Fueling it all is public perception. People are constantly judging you when you have diabetes, and it impacts my perception of myself.
Although I have worked through many of my anxieties regarding my diabetes thanks to my incredible care team, I still worry. Even with great control, my glucose levels can be unpredictable at times. This work represents my anxieties at their worst, but with time, medication, and support from my loved ones, I can be bigger than my fears.
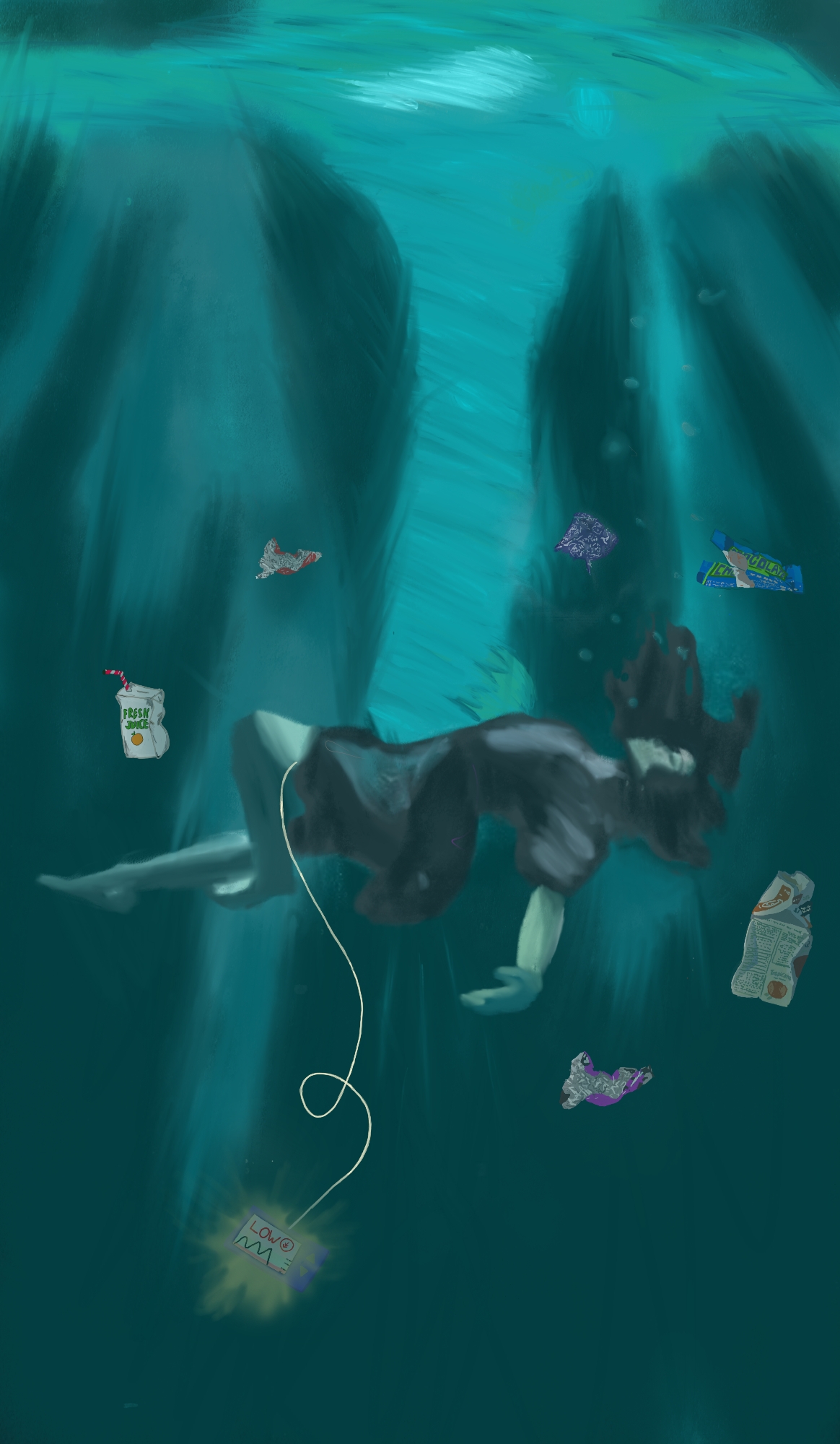
Drowning
Hannah Böhm, Germany
The piece was inspired by the anxiety you get from a really low blood sugar. The person in the picture is struggling for their life, being in a trance, feeling like they could sink to the ground every second. The insulin pump, although shining bright in the dark, is not helping in that moment but rather feels like extra weight. The trash the person is surrounded by is all food you would typically consume during a low blood sugar, like juice or a chocolate bar. It being trash shows that the person already tried their best to get their blood sugar under control, but still did not manage to be okay again.
It also shows the amount of food people with diabetes consume when they are scared of their blood sugar dropping, and like trash in the ocean, it is something that feels wrong and sort of out of place in its environment. It also shows that the person is struggling so much that they don't have the energy to clean up after themselves, but rather the trash floating around them makes them feel even worse.
All in all, this piece shows my perspective on what low blood sugar feels like and the anxiety that comes with it.
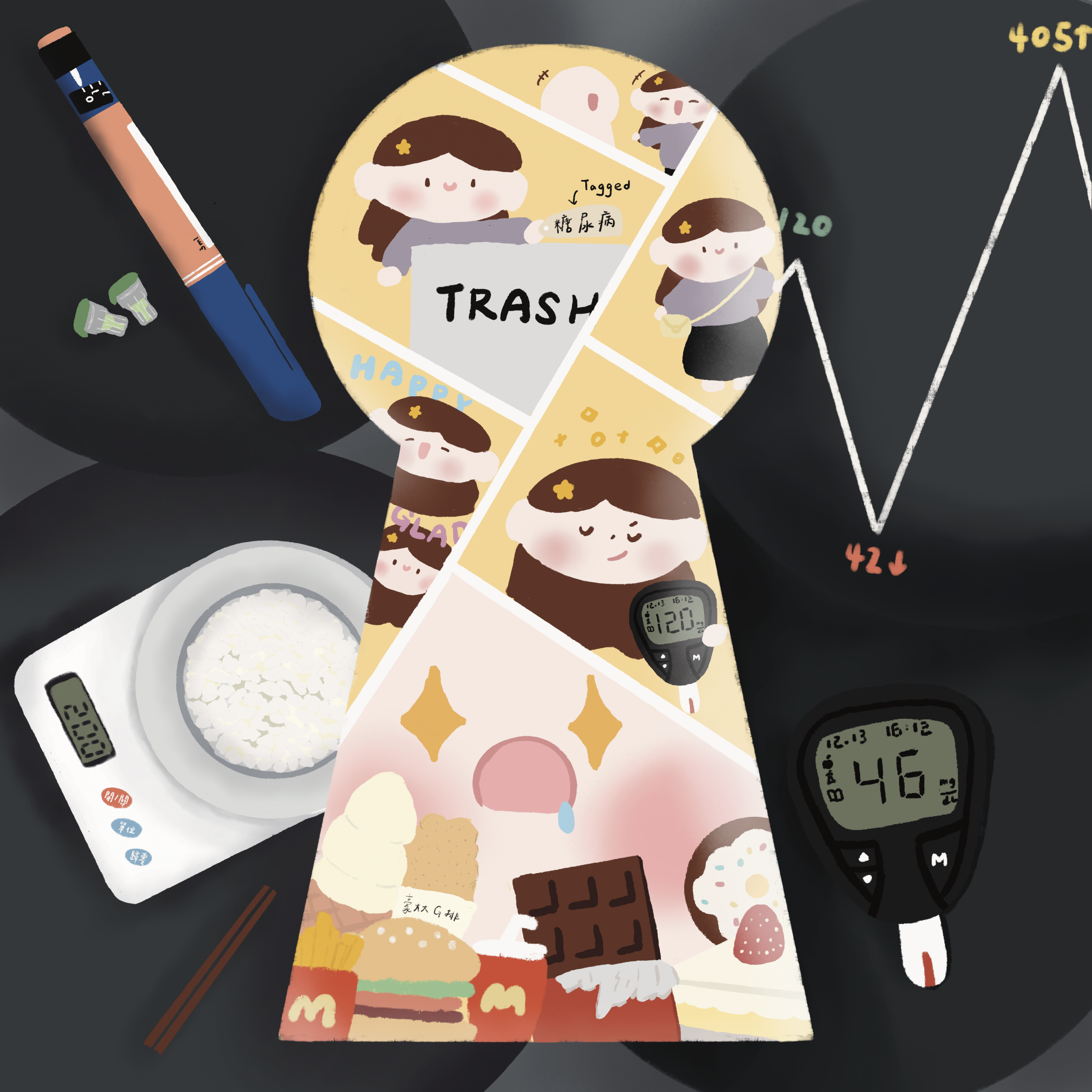
The Keyhole
林宇芹, Taiwan
Through the composition of a keyhole, we glimpse a small universe framed by illness. Blood glucose meters, insulin pens, food scales, and sweets together form the everyday life of someone living with diabetes.
Within this seemingly gentle world lies an undercurrent of anxiety about self-control and a deep longing for freedom. Behind every smile is a silent tug-of-war between numbers and desire.
The keyhole symbolises a life under observation, but also the boundary we face within ourselves — a line that separates sweetness from pain, freedom from restraint, outward understanding from inner truth.

To My Dear Pancreas and Brain
Sara Mariana Meléndez Barrón, Mexico
“The Inner Garden and the Sweet Burden”
When the sweet threshold of childhood closed, I watched my brother take up his cross of sugar. I thought the battle lived only in the whispers of his veins — a chemical secret that would never reach the sanctuary of the mind. I never imagined that my own beginning would be an awakening beyond glucose, a confrontation within the citadel of my spirit.
The day the doctor pronounced the verdict of diabetes, my soul did not fear the needle but the echo that resonated through the dark corridors of my anxiety and depression. My anxiety — whom I’ve named Lucy — unfurled her shadowed wings, soaring toward a horizon of imagined possibilities, veiled in the mist of a future that did not yet exist. I felt disarmed, a spectator before the catastrophe orchestrated by my own mind.
Eight years have carved this path of mine. Today, when I look at Lucy, I no longer see an intruder. I’ve learned that my anxiety is, in truth, my vigilant essence — a nervous sentinel calling out warnings to truths my daily distractions drown out. This new alliance has forged a strange peace between us. I came to understand that we both dwell within my inner garden, and that our coexistence does not deny the possibility of serenity.
I know that not every murmur of the mind is an oracle of truth. The support woven from the threads of familial love, the science of my doctors, and the light of my therapists became my beacon. I discovered the strength that comes from naming the shadow that follows me.
And there, in the embrace of that understanding, I found my greatest blessing — the purest act of love toward myself: to accept my burden and fight not against it, but with it, for a life clothed in peace.

Is This Me?
Jaylen MM, Canada
In June 2023, I was diagnosed with Type 1 Diabetes. I was in my senior year of high school, preparing for university, when my life was turned upside down after a week-long stay in the hospital.
I went from being someone who never really questioned what I ate or where I went too being terrified and hyper-focused on every little detail of my life. My own anxiety prevented me from living. From fears of going low and not being able to get help, all the way to fears of running out of insulin. I laid awake at night knowing there are jobs I won't be able to have. Knowing there are places I can never live because they do not see how insulin is interchangeable with life support.
I often question who I would be without diabetes. I spend endless nights staring into mirrors wondering what I would look like. How care-free would I be. How much easier my life could be. The anxiety eats at me day by day, making me spiral deeper and deeper into an endless barrage of "what if" questions. Who am I? Who was she? Is This Me?

Sleeping Awake
Marcia Bottino, Urugway
Being the mother of a child with Type 1 diabetes makes me feel as though I sleep while awake. I never know if I’ve truly rested, as I’m always watching over his levels, making sure he’s all right. My peace lies in knowing that he’s well, even when anxiety keeps me from sleeping.
His strength in facing this reality inspires and motivates me every single day. The artwork is created in a circuit format, as colouring it helps to ease and balance my anxiety.
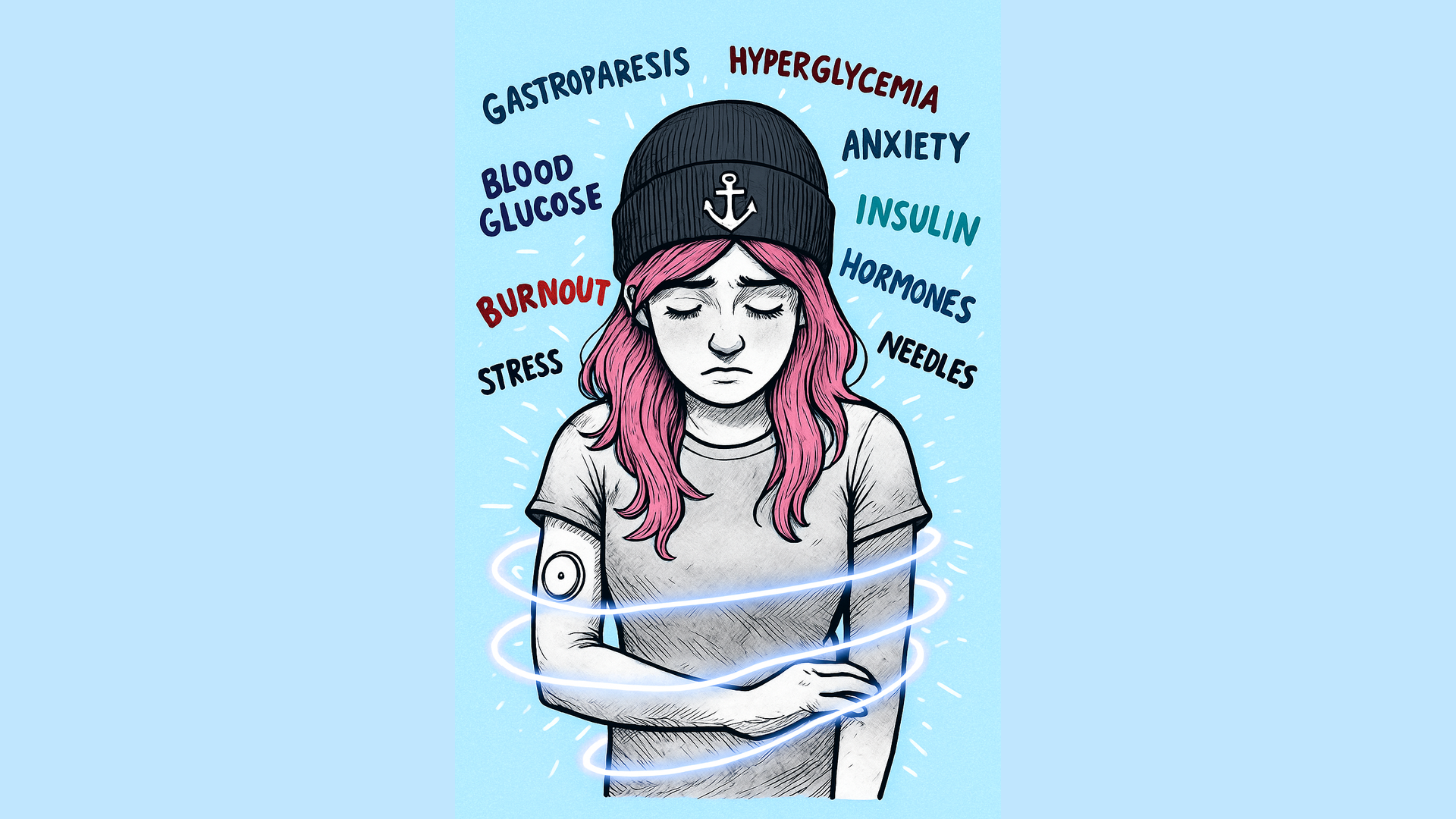
Wrapped in Worry
Stefanie Hilbeck, Germany
This artwork represents the feeling of being bound by fears and worries — the invisible ties that sometimes come with living with diabetes. The glowing lines symbolize the cycle of anxiety that can feel impossible to break.
For me personally, gastroparesis, a complication of diabetes, is one of my greatest fears. It is unpredictable and causes immense suffering for those affected. The constant alarms from sensors or pumps can rob you of sleep and peace of mind, leaving your nerves on edge.
During hypoglycemia, there’s often the terrifying thought that it could be fatal — and that fear lingers. There are so many aspects of diabetes that can cause fear and exhaustion, both mentally and physically.
This image gives form to that weight — to the quiet moments when the struggle feels overwhelming, yet unseen by others.

Through the Tunnel of Struggle
Marwa Kicha, Morocco
This painting powerfully symbolizes the challenges faced by people living with diabetes and their determination to keep moving forward despite them. The dark tunnel represents the difficulties, fears, and uncertainty that often accompany the disease, the daily monitoring, dietary restrictions, and emotional burden. The deep blue tones evoke the sense of isolation and struggle that many patients experience as they navigate their condition.
However, at the end of the tunnel, there is a radiant light, a symbol of hope, strength, and perseverance. The small figure walking toward the light represents the diabetic patient who refuses to give up, continuing their journey with courage and faith. The reflection of the light on the path suggests that even in darkness, their efforts and resilience illuminate the way forward.
In essence, this artwork captures both the pain and the power of endurance, showing that, despite the hardships, there is always a path toward healing, balance, and inner peace.

Say cheese! A portrait of my social anxiety
Sharron Fidler, United Kingdom
When I am smiling but dying inside.
My work is based on my mental health and how I portray myself to the world. This piece is called "Say cheese! A portrait of my social anxiety" I have only in the last year begun to create using oils and my confidence has gained ground. I have been diabetic for over 25 years and struggle with being present in my treatment, being able to create gives me hope for my future

Tip of it
Louise Richardson, United kingdom
The “Tip of it” was made in response to my daughter's diagnosis at 10 of type 1 diabetes. The diagnosis is a shock and the condition is intrusive, repetitive and has to become deeply embedded into all daily activities. The only way to monitor the condition was for her to prick her finger to monitor blood glucose levels, around six to eight times a day. This, on its own, was difficult.
The “Tip of it” was based on a year's worth of finger pricks - it became a visual calculation which seemed to tell a story more than words. Diabetes is a very number-driven condition, blood glucose readings, carbohydrate counting units of insulin HbA1c (measurement of blood glucose over a three-month period).
The “Tip of it” is in no way a comparison to what my daughter has to go through but somehow helped to visualise the process reflecting the time and the physicality of the process the aggressive action of pushing the pins into the gloves was particularly difficult - I wore a skin coloured plaster on my finger throughout the whole process which became more and more scarred - beginning to resemble the surface of my daughters fingers. The piece is made from fine gloves and pins representing years' worth of finger pricks.

Inside and outside the circle of life
Ana Jurić, Bosnia and Herzegovina
The submitted painting was made using oil on canvas technique. The dimensions are 40 x 60 cm. It's inspired by my everyday life...I'm the mother of two wonderful teenage girls diagnosed with DM 1. We have lived with diabetes for 7 years, and we went through various stages of life with DM 1, but my struggle with anxiety is constant after I once experienced acute stress disorder under the influence of stressful life. Regardless of the struggle that takes place outside the blue circle of life, I do my best so that my daughters don't feel that their diabetes has any negative impact on our lives. I'm learning to embrace and love life, to appreciate simplicity and to practice gratitude. By looking at them and admiring their smiles, I also heal and learn how to overcome all obstacles...Life is not what happens to you but how you decide to accept it...or not.
The painting shows me and my daughters, and I'm the author. I'm not a professional artist; I'm an amateur who enjoys art.

Diabetes labyrinth
Ariadna Castrellón Calzada, Mexico
The illustration captures the profound 'diabetes distress.' It illustrates the exhaustion of constant monitoring (devices, syringes) and the psychological struggle (the spectral figure, the 3:00 AM time) that torments those living with this condition. The vigilant adult figure underscores the burden of care and family concern. In the center, a winding river of peaks and valleys symbolizes the unpredictable and obstacle-filled path that generates intense daily anguish, alongside the constant desire to live and enjoy everything life offers. I am the mother of a young man who has recently been diagnosed.

The Weight of Choices
Vittoria di Benedetto, Italy
I found out I had Type 1 diabetes when I was 25. Beyond the initial shock, I didn’t make a tragedy out of it — I learned to accept it over time, not that I had much choice.
But there has always been one thing that drives me mad, that triggers my anxiety and sometimes even real episodes of depression (which I’ve struggled with for much longer). No matter how many checks I do, how many devices I use, how carefully I follow my diet and all the sacrifices I make, this condition often slips out of my control — doing whatever it wants and leaving me wondering why all my efforts end up wasted.
The anger, anxiety, and frustration sometimes make me want to stop taking care of myself, to throw everything away and just let whatever happens, happen. But I can’t. So I keep going — holding on to hope for the future and for better ways to manage my life.

Tragically Beautiful
Chloe Moon, Australia
Three months ago, our world shifted when our three-year-old son was diagnosed with Type 1 Diabetes. The experience was terrifying and heartbreaking—an avalanche of emotions and information all at once. T1D is one of those conditions you don’t truly grasp until you’re living it. Its seriousness, its unpredictability, and the way it reshapes everyday life—it’s overwhelming.
We’re incredibly grateful we caught it in time. Our hospital visit could have ended in the ICU—or worse. That thought still chills me. Every day since has been a learning curve. Some days are harder than others, but through it all, I’ve been in awe of our son’s resilience. At just three years old, he’s faced this challenge with a strength that humbles me.
I’ve tried to put into words the anxiety that comes with every blood sugar fluctuation, every injection before a meal, every moment he’s asked to finish food he may not want—because the stakes are so high. But the truth is, I can only speak from my perspective as his mum. I’ll never fully understand what it feels like for him. I just know I’ll be beside him every step of the way.

Tread Lightly (This Is Anxiety)
Shelby Dillingham, United States
Tread Lightly (This Is Anxiety) is a sculptural self-portrait in the language of chronic illness, ecofeminism, and resistance. I constructed this piece using my own recycled medical waste — thousands of used needles — embedded into platform Doc Martens, a symbol of defiance and identity. These boots are unwalkable, painful, and threatening — and that is the point.
As a Type 1 diabetic, my survival is dependent on a daily ritual of piercing, monitoring, injecting. These acts are intimate and clinical, invisible to most — but here they take center stage, made grotesquely visible. Every needle carries the memory of a moment, a cost, a calculation. The physical weight of the piece mirrors the financial and emotional toll of living with a disease that never ends, never rests, and is never free.
The oceanic background speaks to vastness, overwhelm, and the deep, unknowable depths of living with anxiety — a constant undercurrent that threatens to pull you under, even on still days.
This is not just a personal narrative. As an ecofeminist, I confront the systems — medical, environmental, capitalist — that create and sustain this kind of suffering. Medical waste, often treated as shameful or disposable, becomes here a material of power and protest. The boots cannot move forward without pain — just as I, and many others, navigate a world where the act of simply continuing is both radical and exhausting.
This is anxiety. This is endurance. This is survival made visible.
Holding myself together
Julia Stefaniak, Poland
My artwork reflects the hidden struggles that many people with diabetes carry every day - burdens that are rarely seen or understood by others. From the outside, everything may look fine, but inside there is constant calculation, fear, and exhaustion. It’s a quiet fight that happens beneath the surface, where numbers and emotions mix in silence.
The piece shows a figure looking at their own reflections - not out of vanity, but out of the need to truly see and care for themselves. Living with diabetes often means learning to be your own protector, to give yourself compassion when others cannot fully understand what you’re going through.
Through layers of shadow and light, I wanted to express both the loneliness and the strength that come from this journey. Anxiety may whisper doubts, but self-awareness and self-kindness can turn that whisper into resilience. My artwork is a reminder that what’s invisible can still be deeply felt - and that caring for yourself is an act of quiet courage.

Fragile Silences
Francesco Pecchia, Italy
This artwork was born from observing how anxiety and diabetes can intertwine silently in everyday life, creating an invisible web of fragility and worry. I was inspired by the desire to transform the perception of this inner weight into a visual language that expresses not only vulnerability but also the strength each of us carries within. The amber light glowing from the chest represents my personal belief that, despite difficulties, there is always a form of resilience capable of illuminating even the most uncertain and melancholic moments.
In this illustration, a stylised human figure sits immersed in a cool, subdued environment. Thin, transparent threads connect symbols associated with diabetes — a glucometer, a syringe, a stopped clock, a grey cloud, and violet flames — representing the constant presence of the condition and the mental burden it brings. The figure’s hand, resting on the chest, emits a warm amber light that contrasts with the melancholy atmosphere, symbolising the inner strength and resilience that endure through the quiet of anxiety.

Colour Flash
Ingo Vieweg, Germany
I’m 41 years old and was diagnosed with Type 1 diabetes four months ago. Painting and drawing help me relax and keep my blood sugar levels stable.
In this piece, I’ve expressed my first experiences with low blood sugar and how I felt at the beginning. It’s painted in acrylic on wood.

Playing with needles
Julie Duquette-B, Canada
Diabetes has been a part of my life for as long as I can remember. The struggle through adolescence and adulthood has been difficult. Realizing that your life depends on one injection after another can be deeply discouraging at times.
My artwork aims to show how unsettling it is to see a child playing with needles—but for a child with diabetes, this is everyday life. We handle needles long before we reach adulthood. We take on responsibilities far greater than our age. I used darker colors to convey feelings of sorrow and anxiety. A child holding a teddy bear and playing with syringes represents the contrast between innocence and illness.
In 2015, when my oldest son was diagnosed, guilt inevitably found its way in. The anxiety reached a whole new level. I hope his journey will be easier than mine.
To everyone living with the highs and lows of diabetes: you are doing an incredible job. If no one has told you this yet—it’s not your fault, and you are doing the best you can. We are so close to finding a cure; hang in there a little longer.
Even though it’s not always easy, life still has so much to offer—and since we already know we won’t live forever, we might as well live to the fullest.

Silent Cry for Help
Nina Emmerich, Germany
I was seven when I was diagnosed — that was in 2003. There were no sensors, no inclusion support at school, no psychologists on the ward — nothing at all.
For years, I thought it was normal for children and teenagers with Type 1 diabetes to be blamed by those around them — told they had ruined their parents’ lives, not allowed to go on school trips, growing up completely cut off from the reality of other kids their age. Because I wasn’t the child Nina — I was my diabetes. A number. And with every number from a glucose test or HbA1c result came the fear of not being good enough, of having failed, of no longer being loved, and of facing even more violence.
On the outside, everything looked perfect. But behind the closed curtains, life was hell. The house screamed, the child screamed, the teenager screamed. Yet no one heard it.
It’s important to me to shed light on experiences like these. I only learned as an adult that this life was anything but normal — and that help actually exists. No child should ever have to grow up with such fears.

Within Me
Roberto Carlos Velazquez Zamora, Mexico
At 25 years old, my brother began to suffer from diabetes. Today, he is learning to live with this change in his life.
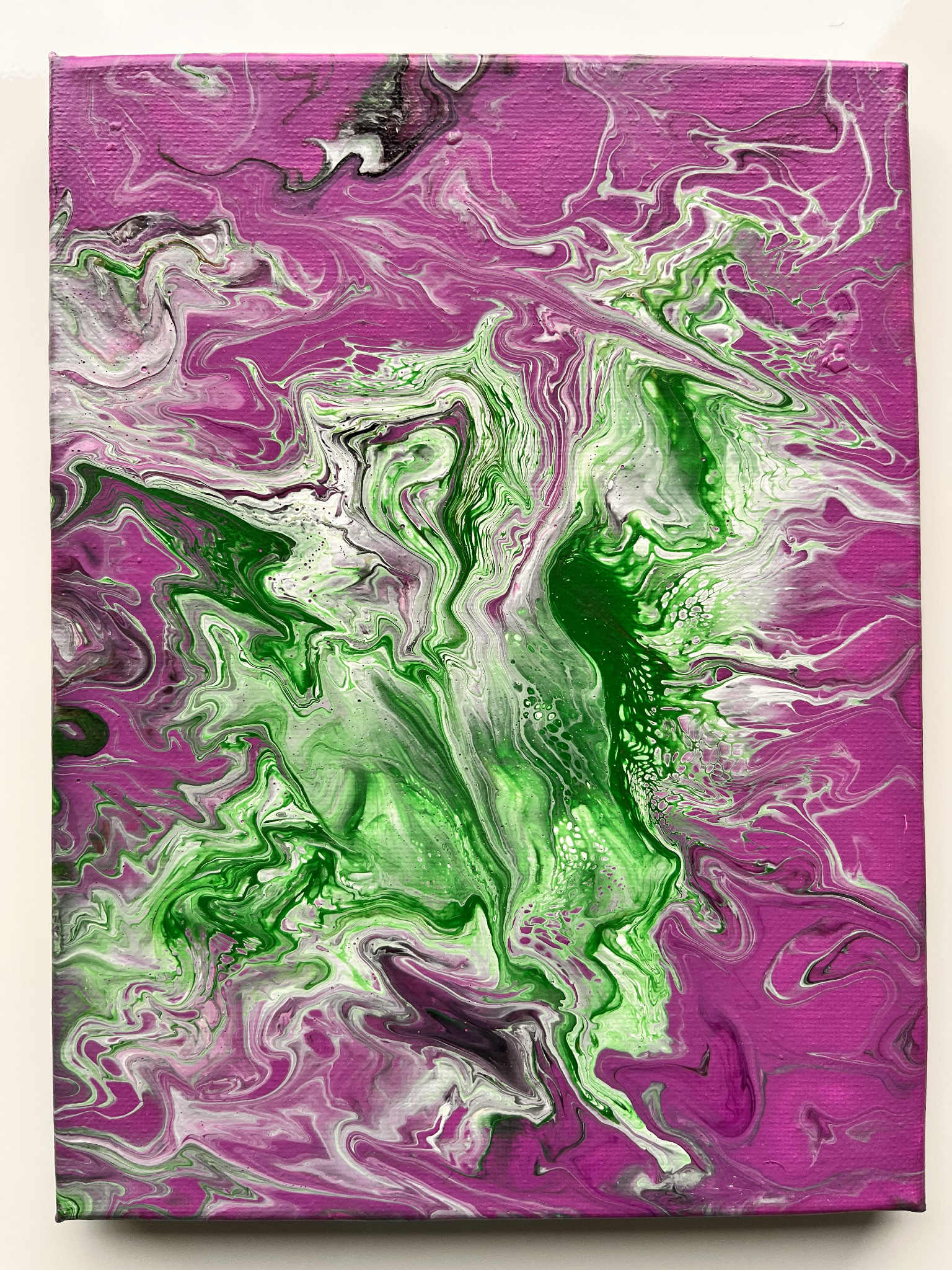
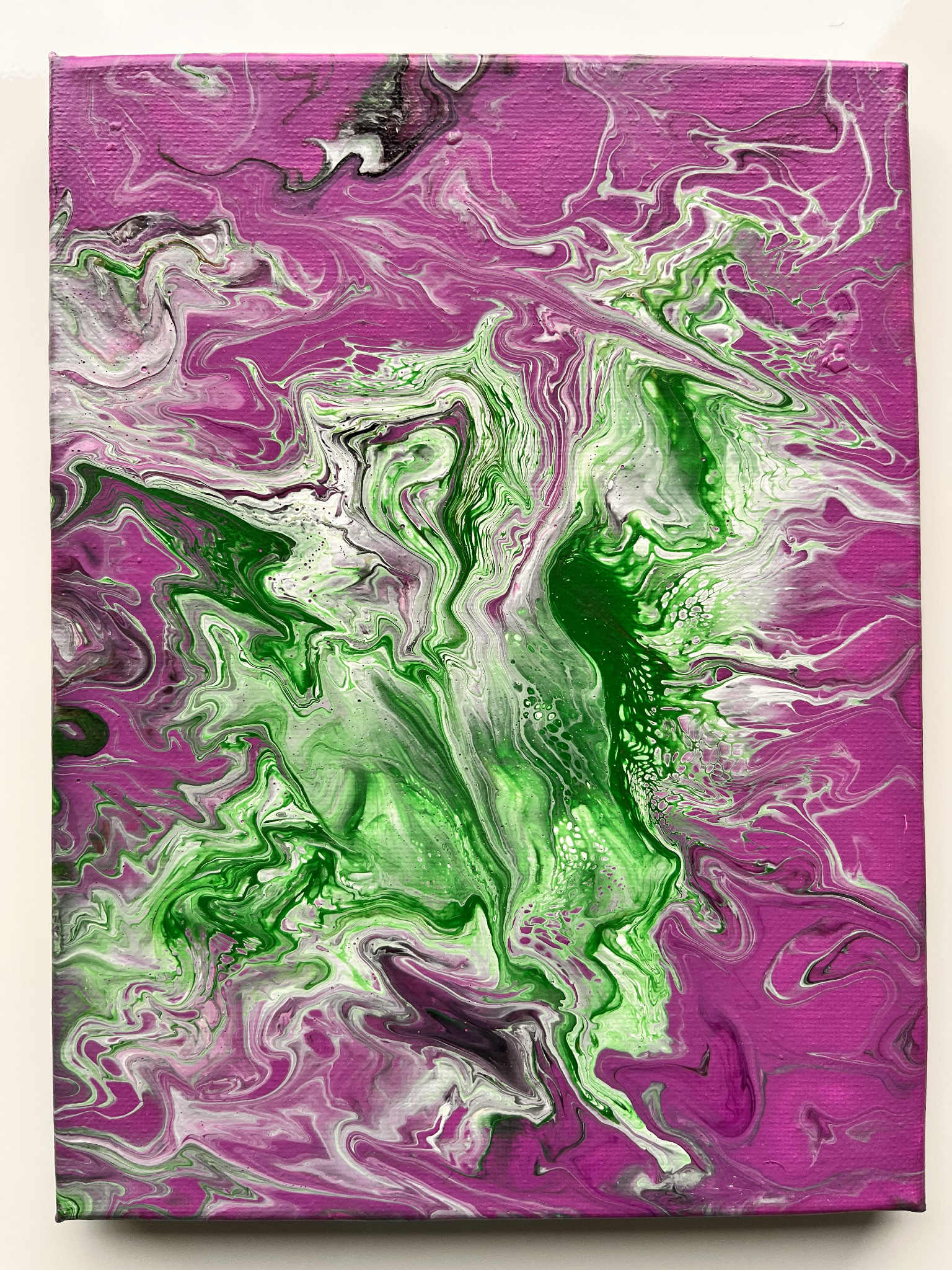
The Battle Within
Daniela Asparuhova Georgieva, Switzerland
This painting was created using the acrylic pouring technique — every line and shape is unique and cannot be repeated. Within it, a dragon and a snake fight each other — a symbol of my inner struggle with myself. This is my world with Type 1 diabetes — a constant balance between control and fear. Every day, I monitor my blood sugar, afraid of both hypo- and hyperglycaemia, yet outwardly I appear calm and smiling. The pink tones show how others see me — as if everything were fine. But the green and dark swirls reveal the truth: the fear, exhaustion, and uncertainty that few ever notice. The slightly blurred effect of the painting reflects how I sometimes see the world when I inject insulin — as if reality itself were dissolving, just like the colours on the canvas.
I’ve lived in Switzerland for ten years. I’m an engineer with a background in education, but I can’t find a job. The language barrier keeps me trapped in a vicious circle: no work means no money for language courses — and without the language, no work. After years of worry and uncertainty, I developed diabetes, which has since progressed to Type 1. This painting reflects my inner struggle — between fear and hope, between control and helplessness.
It is unique because I poured my pain and my hope into it.
“This is me — between dragon and snake, between fear and strength. This is my diabetes.”
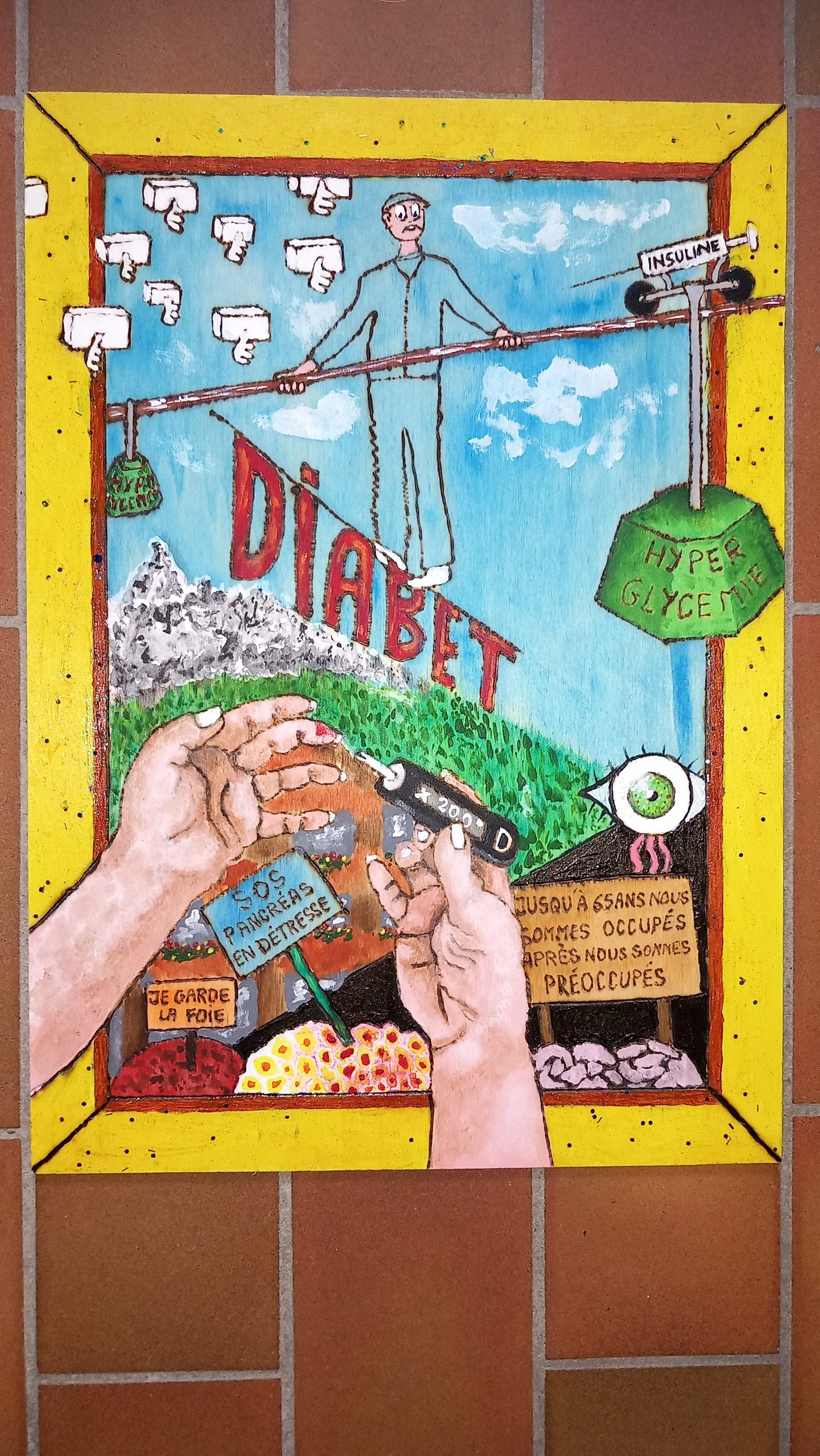
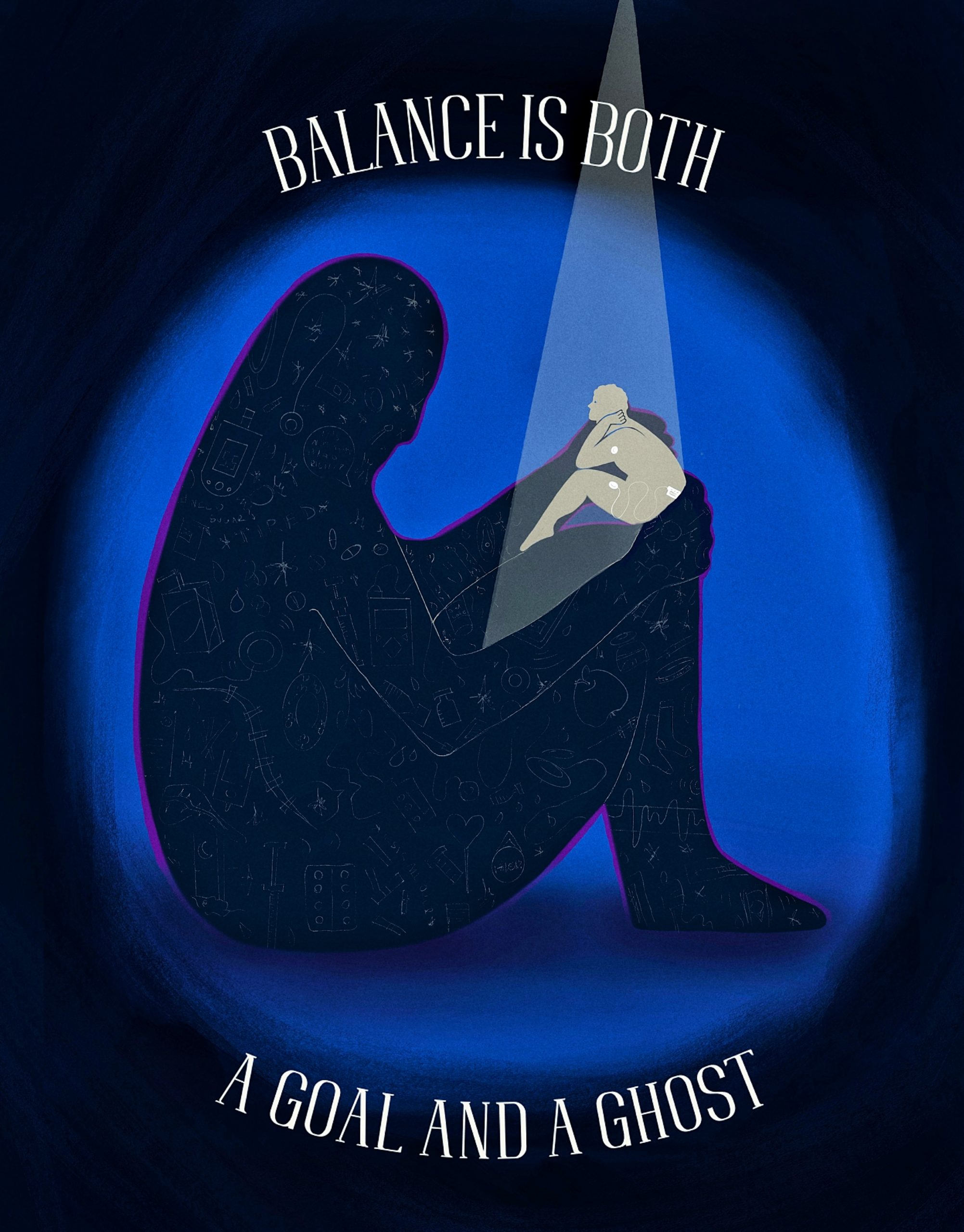
Diabetes Is a Matter of Balance
Kongchai Bernard, Switzerland
The intention was to depict the distress of our organs, and then to give wings to the pieces of sugar so that they could escape the allegory of this painting.
SELECT AND DOWNLOAD INDIVIDUAL COLORING PAGES